
Psychedelic-assisted Therapy Using Ketamine for Cancer Patients
by PNI Experts
Cancer patients may find relief from mental anguish with ketamine-assisted therapy available at Saint John’s Health Center and Pacific Neuroscience Institute ® (PNI).
The diagnosis of cancer, particularly terminal illness is devastating. Along with the physical ravages of the disease, patients must deal with the mental stress that their disease inevitably causes.
Medical psychedelic-assisted therapy using ketamine is a relatively new treatment approach that is being used for treating people with mental anguish conditions, including depression, anxiety, and PTSD. In recent years, research has also begun to explore the potential benefits of ketamine in the treatment of cancer-related symptoms, such as pain, fatigue, and depression.
Ketamine is a medication that has been shown to have rapid antidepressant and anti-anxiety effects, which can be beneficial for patients who are dealing with the emotional and psychological stress of a cancer diagnosis and treatment. While medical experience in this area is still relatively new, and more studies are needed to determine the safety and efficacy of ketamine-assisted therapy for cancer patients, physicians at Pacific Neuroscience Institute® (PNI) and Providence Saint John’s Health Center, believe there are many potential benefits that patients with cancer can experience. It’s important to note that ketamine is only administered under the care of a medical professional and in a controlled clinical setting.
Easing the way with ketamine
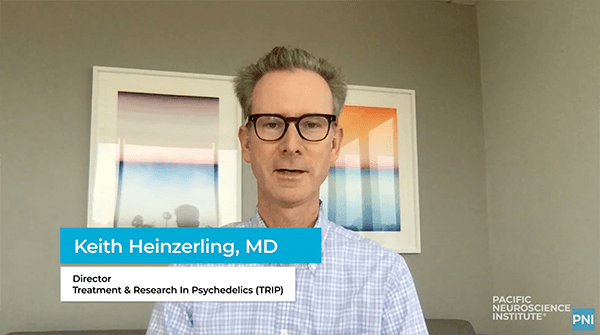
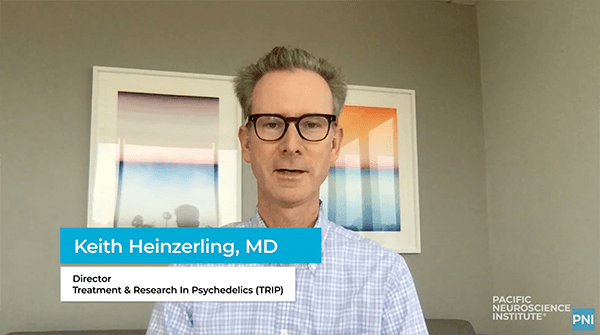
Keith Heinzerling, MD, an internal medicine and addiction medicine specialist, and Director of the Treatment & Research In Psychedelics (TRIP) program at PNI, treats patients with ketamine with a psychedelic-assisted approach. “Usually, ketamine treatment includes one or a few in-clinic ketamine dosing sessions under clinician supervision integrated with preparatory and integration counseling over the period of a few months,” Dr. Heinzerling explains.

At Saint John’s, Przemyslaw W. Twardowski, MD, a medical oncologist and Director of Clinical Research, Urology, and Urologic Oncology, takes care of patients with prostate, bladder, kidney, and testicular cancers. Dr. Twarowski, in practice for over 20 years, adopts the philosophy of providing his patients with compassionate, high-level cancer treatment. Each person’s circumstances and values are unique and ketamine-assisted psychedelic therapy represents another tool he can offer his patients.
FAQs about ketamine therapy for cancer patients
Q: How does ketamine work in the body?
A: Ketamine is a dissociative anesthetic that works by blocking NMDA receptors in the brain, which can lead to a change in consciousness and a dissociative state. This is thought to be the mechanism by which ketamine can produce rapid and robust antidepressant effects.
Q. How is ketamine administered?
A: At PNI, ketamine is given as an IV intramuscular injection.
Q: How long is a ketamine-assisted psychedelic treatment?
A: The full psychedelic-assisted ketamine treatment includes one to two 1-hour preparatory psychotherapy counseling sessions, the clinician-supervised dosing session which lasts about 3 hours, and several 1-hour integration sessions. The total duration can be 3 to 6 months and is mutually determined by the counselor and patient.
Q: What is the difference between ketamine and other psychedelic-assisted therapies?
A: Ketamine is approved by the Food and Drug Administration (FDA) as a dissociative anesthetic and in lower doses, it produces psychedelic effects. Other ‘classic’ psychedelics (such as LSD or psilocybin) are serotonergic psychedelics. These drugs work by activating the serotonin receptors in the brain, which can lead to changes in perception, mood, and cognition. The dissociative and psychedelic effects of ketamine are thought to be mediated by its action on NMDA receptors, rather than serotonin receptors.
Q: What are the potential benefits of ketamine-assisted therapy for cancer patients?

A: There is still limited research on the use of ketamine in cancer patients, but initial studies have suggested that it may be effective in reducing symptoms of pain, fatigue, depression, anxiety, and existential dread. Used in a psychedelic-assisted approach under the supervision of trained medical experts, ketamine can induce a sustained state of well-being and hopefulness. Additionally, ketamine may have anti-inflammatory properties, which may be beneficial in cancer patients.
Q: What are the potential risks and side effects of ketamine-assisted therapy?
A: As with any medication, there are potential risks and side effects associated with ketamine use. Some of the most common side effects include drowsiness, dizziness, and confusion. Additionally, ketamine can cause changes in blood pressure and heart rate, which can be dangerous for individuals with heart or blood pressure problems. Long-term use of ketamine can also lead to addiction and cognitive impairment.
Q: Is ketamine-assisted therapy FDA-approved for the treatment of cancer-related symptoms?
A: Ketamine is FDA-approved as an anesthetic and for certain neurological conditions, but it is not currently approved for the treatment of cancer-related symptoms. However, as research on ketamine’s potential benefits in cancer patients continues, it is possible that the FDA may consider approving it for this use in the future.
Q. Is ketamine-assisted therapy covered by insurance?
A. Preparatory and integration counseling sessions may be covered by insurance, while at this time, the dosing session is $1200 and is considered an out-of-pocket expense, until FDA approval.
Ketamine-assisted therapy for cancer patients is still experimental, and more research is needed to fully understand the potential benefits and risks of this treatment approach. As with any medical treatment, individuals considering ketamine-assisted therapy should discuss the potential benefits and risks with their healthcare provider.
More information:
Ketamine Treatment: 310-582-7612 | Clinical Trials: 310-582-7611
About Dr. Keith Heinzerling

Keith Heinzerling, MD, practices internal medicine and is an addiction medicine specialist at the Pacific Brain Health Center, Pacific Neuroscience Institute. His clinical and research focuses are on the treatment of alcohol, drug, and substance use problems, with anti-addiction medications. As director of the Treatment & Research In Psychedelics (TRIP) program, he is involved in the development of psychedelic-assisted therapies for those suffering from addiction, depression, anxiety, and PTSD. He is the principal investigator of clinical trials using psychedelic-assisted therapy tackling conditions including alcohol use disorder, major depression, and generalized anxiety disorder. Dr. Heinzerling is a trained psychedelic guide and holds a Certificate in Psychedelic-Assisted Therapies and Research (CPTR) from the California Institute of Integral Studies (CIIS).
About Dr. Przemyslaw Twardowski
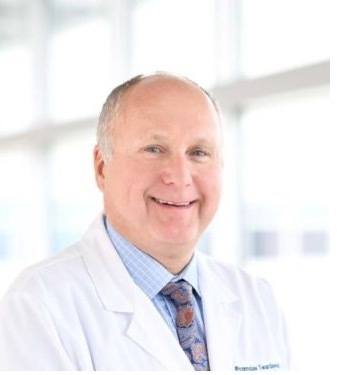
Przemyslaw Twardowski, MD, is a board-certified medical oncologist, who has vast experience in the management of genitourinary malignancies including prostate, bladder, kidney, and testicular cancers. Over the last 20 years, he was a principal investigator and contributor to multiple clinical trials that expanded treatment options for patients with cancers of the genitourinary tract. Dr. Twardowski is a member of the American Society of Clinical Oncology and was selected as one of America’s Top Doctors multiple times. He has published more than 100 scientific articles, abstracts, and book chapters and he lectures nationally and internationally. Dr. Twardowski’s medical philosophy is to provide compassionate, state-of-the-art cancer treatment always taking into account each patient’s unique circumstances and values.
Useful Links
- Treatment & Research In Psychedelics (TRIP)
- Anxiety Research Study
- Ketamine Assisted Therapy Program
 Psychedelic-Assisted Therapy with Ketamine at PNI
Using ketamine in a psychedelic-assisted approach, we treat people 16 years and older who are treatment-resistant or who wish to effectively tackle deep-rooted, unresolved trauma that has not been adequately…
Psychedelic-Assisted Therapy with Ketamine at PNI
Using ketamine in a psychedelic-assisted approach, we treat people 16 years and older who are treatment-resistant or who wish to effectively tackle deep-rooted, unresolved trauma that has not been adequately…
 Think Neuro Podcast: The Promise of Psychedelics | Dr. Keith Heinzerling & Louie Schwartzberg
Addiction and depression are two of the most widespread conditions in all of medicine. After decades of research, doctors are still looking for alternatives for when medication and cognitive training…
Think Neuro Podcast: The Promise of Psychedelics | Dr. Keith Heinzerling & Louie Schwartzberg
Addiction and depression are two of the most widespread conditions in all of medicine. After decades of research, doctors are still looking for alternatives for when medication and cognitive training…
 Meet Dr. Heinzerling
Dr. Heinzerling is the Director, Pacific Treatment & Research In Psychedelics Program; Internal Medicine – Addiction Medicine, Brain Health Center. He practices internal medicine and is an addiction medicine specialist…
Meet Dr. Heinzerling
Dr. Heinzerling is the Director, Pacific Treatment & Research In Psychedelics Program; Internal Medicine – Addiction Medicine, Brain Health Center. He practices internal medicine and is an addiction medicine specialist…
 Psychedelic-Assisted Therapy at Pacific Neuroscience Institute
Dr. Keith Heinzerling is an addiction medicine specialist and Director of Treatment & Research In Psychedelics (TRIP) at Pacific Neuroscience Institute in Santa Monica, CA. Learn about how psychedelic-assisted therapy…
Psychedelic-Assisted Therapy at Pacific Neuroscience Institute
Dr. Keith Heinzerling is an addiction medicine specialist and Director of Treatment & Research In Psychedelics (TRIP) at Pacific Neuroscience Institute in Santa Monica, CA. Learn about how psychedelic-assisted therapy…

Psychedelic-Assisted Therapy with Ketamine at PNI

The Promise of Psychedelics | Dr. Keith Heinzerling & Louie Schwartzberg

Meet Dr. Heinzerling
Psychedelic-Assisted Therapy at Pacific Neuroscience Institute
About the Author
PNI Experts
Last updated: April 4th, 2024