

2017 International Stroke Conference (ISC)
by Jason Tarpley
HIGHLIGHTS

February 21-24, 2017: Stroke’s biggest meeting hosted by the American Heart Association was recently held in Houston, TX, to share and debate the latest science in ischemic and hemorrhagic stroke. This year’s meeting highlighted more big wins for the treatment of ischemic stroke and brain aneurysms. On the other hand, the latest trial in intracerebral hemorrhage (ICH) again disappointed our community pointing out the need for more work in ICH. Here are some of our selected highlights from this year’s very exciting meeting.
Ischemic Stroke – Endovascular Therapy (EVT) results dominated the Ischemic Stroke Landscape this year
- Big Uptick in EVT since MR CLEAN trial. A very large Get with the Guidelines (GWTG) database from all Comprehensive Stroke Centers showed an increase in usage of EVT since publication of the first trial of thrombectomy in late 2014. For patients arriving to hospital <4.5 hours with NIHSS >/= 6, EVT was given in 9% of these patients in Q2 of 2003 and in 27.3% in Q3 of 2016.
- M2 occlusions and EVT – EVT for M2 occlusions is very common practice. In fact 23% of all thrombectomies in the Trevo Worldwide Registry were done for M2 occlusions.
- Even large volume infarcts benefitted from EVT. In pooled data from 6 trials, core infarct volume (obstruction of the blood supply) was a strong predictor of outcome. However, even patients with large infarcts at the time of EVT benefitted from treatment.
- Thrombectomy after 6 hours – Selected patients with large vessel occlusions who present to the hospital after 6 hours but are appropriate for treatment consideration are now very often treated and derive significant benefit from EVT.
Cerebral Aneurysms – Flow diversion and more
- Flow Diversion of aneurysms with the Pipeline device has already shown impressive safety and efficacy in large aneurysms. Data from the PREMIER Trial now shows that Pipeline turns out to be very safe and effective for small aneurysms too. Flow Diversion was also shown in a meta-analysis presented at ISC to be the most effective way to preserve vision in aneurysms that compress the optic nerve.
- GREAT Trial – The latest generation of HydroCoils outperformed traditional platinum brain aneurysm coils when it comes to a composite outcome at 18 months.
- New devices for treating aneurysms showed early promise. Small trials for Pulserider and WEB devices showed safety relative to existing devices.
Notable Negatives:
- HeadPoST TRIAL – Head position up vs. flat made no difference for hemorrhagic or ischemic stroke patients
- SPOTLIGHT Trial – No benefit to NOVO-7 when given to intracerebral hemorrhage patients, even when CTA spot sign is present.
STUDY UPDATE DETAILS
PREMIER Trial – Flow Diversion
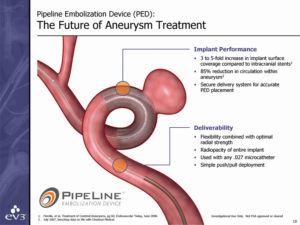
The Pipeline Embolization Device (PED; Medtronic) depicted here is placed in the artery to divert blood flow away from an aneurysm. It had already been shown to work for 1.2 cm and larger aneurysms. In the PREMIER trial, aneurysms of less than 1.2 cm were treated with pipeline. In fact, 84% of the aneurysms treated in this trial were less than 7mm. Major stroke or death was observed in 2.1% and 0.7 % of patients treated with Pipeline. In this study there were no intra-operative aneurysm ruptures and only 2.2% of aneurysms required retreatment at 1 year. Even more utility of flow diversion was demonstrated in a meta-analysis of patients with large paraclinoid aneurysms resulting in optic nerve compression. In this meta-analysis endovascular flow diversion was better at preserving and improving vision than other available other current strategies such as coiling or open clipping.
GREAT Trial – A trial of hydrogel coils for brain aneurysms
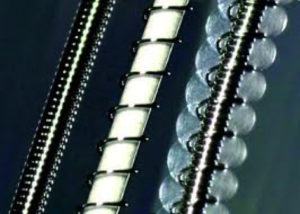
Brain aneurysms are typically treated by filling them with platinum coils. The fuller of coils an aneurysm is, the more complete its cure. Hydrogel coils are strands of platinum with gel around them. This gel expands when in contact with the blood which allows for tighter packing or more complete filling of the aneurysm. The GREAT trial presented their latest data on the newest generation of these coils which are softer and easier to work with than the previous generation. This new generation of hydrogel coils resulted in an improved outcome compared with traditional platinum coils. The composite outcome was 18-month disability, aneurysm recurrence, need for aneurysm retreatment, and any significant morbidity or mortality. The effect seems to be largely driven by lower rates or recurrence and retreatment in the hydrogel coil arm of the trial.
Thrombectomy after 6 hours
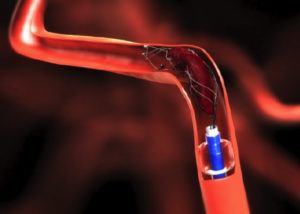 Many patients are treated with thrombectomy beyond the typical 6-hour time window. These patients are selected for treatment outside of the typical 6-hour window based on complex methods which typically include perfusion imaging (see color maps below). At ISC this year, we saw in the Trevo worldwide registry that fully 1/3 of thrombectomy patients received treatment in the > 6 hr time window and 1/5 of the thrombectomy patients in the Providence GWTG database were treated at greater than 6 hours. Patients treated in this delayed time window had worse discharge ranking scores but had no worse NIH stroke scale, length of stay. These data suggest that properly selected patients in the delayed time window derive almost as much benefit as patients treated in the early time window. Our research was presented as one of two studies detailing stroke transfer times and outcomes in data from 562 acute ischemic stroke patients with large vessel occlusions and is described in Clinical Neurology News.
Many patients are treated with thrombectomy beyond the typical 6-hour time window. These patients are selected for treatment outside of the typical 6-hour window based on complex methods which typically include perfusion imaging (see color maps below). At ISC this year, we saw in the Trevo worldwide registry that fully 1/3 of thrombectomy patients received treatment in the > 6 hr time window and 1/5 of the thrombectomy patients in the Providence GWTG database were treated at greater than 6 hours. Patients treated in this delayed time window had worse discharge ranking scores but had no worse NIH stroke scale, length of stay. These data suggest that properly selected patients in the delayed time window derive almost as much benefit as patients treated in the early time window. Our research was presented as one of two studies detailing stroke transfer times and outcomes in data from 562 acute ischemic stroke patients with large vessel occlusions and is described in Clinical Neurology News.
Perfusion Imaging and Thrombectomy
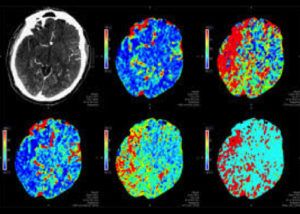 In a pooled analysis of six thrombectomy trials, Dr. Bruce Campbell’s group showed that perfusion imaging combined with RAPID software strongly predicted outcome after thrombectomy. Specifically, patients who had thrombectomy had worse outcomes if they showed larger area of core infarct on perfusion imaging prior to their treatment. However, even for large volume infarcts at the time of thrombectomy, there was significant benefit to receiving the thrombectomy.
In a pooled analysis of six thrombectomy trials, Dr. Bruce Campbell’s group showed that perfusion imaging combined with RAPID software strongly predicted outcome after thrombectomy. Specifically, patients who had thrombectomy had worse outcomes if they showed larger area of core infarct on perfusion imaging prior to their treatment. However, even for large volume infarcts at the time of thrombectomy, there was significant benefit to receiving the thrombectomy.
Thrombectomy for M2 occlusions
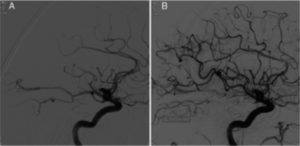 Many trials show that endovascular therapy (EVT) works to treat occlusions of the internal carotid artery or the M1 branch of the middle cerebral artery (MCA). AHA Guidelines suggest it might be reasonable to consider emergent EVT on more distal occlusions like M2 and M3 branch occlusions of the MCA. The Trevo Registry shows us that in real world practice, 23% of all thrombectomies are done for patents with M2 MCA occlusions. The figure shows restored blood flow in one such M2 occlusion before (A) and after (B) EVT.
Many trials show that endovascular therapy (EVT) works to treat occlusions of the internal carotid artery or the M1 branch of the middle cerebral artery (MCA). AHA Guidelines suggest it might be reasonable to consider emergent EVT on more distal occlusions like M2 and M3 branch occlusions of the MCA. The Trevo Registry shows us that in real world practice, 23% of all thrombectomies are done for patents with M2 MCA occlusions. The figure shows restored blood flow in one such M2 occlusion before (A) and after (B) EVT.
Other top news from the ISC meeting can be found on the conference website.

Jason W. Tarpley, MD, PhD is a board-certified neurologist with fellowship training in vascular neurology. He is director of the Pacific Stroke & Aneurysm Center and specializes in ischemic and hemorrhagic stroke, cerebral aneurysms, and carotid artery stenosis.
About the Author

Jason Tarpley
Jason W. Tarpley, MD, PhD, is a board-certified neurologist with fellowship training in vascular neurology. He is director of the Pacific Stroke & Aneurysm Center and specializes in ischemic and hemorrhagic stroke, cerebral aneurysms, and carotid artery stenosis.
Last updated: August 2nd, 2019