

Stop & Smell the Roses: Experiencing a Brain Aneurysm
by Guest Author
A South Bay man survives a life-threatening brain aneurysm thanks to a rapid medical response at Providence Little Company Medical Center in Torrance, California.
Charles Demachy, a local SoCal plant nursery owner, remembers the headache most of all. It was crushing and “weird,” he says. En route to Providence Little Company of Mary Medical Center Torrance, he recalls feeling like there was bleeding inside his head. There was.
A Ruptured Brain Aneurysm
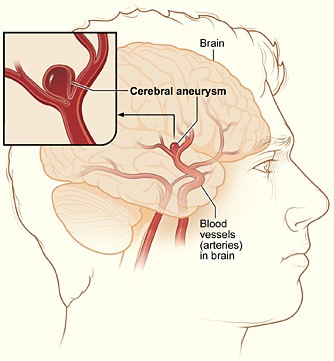
Demachy had a ruptured brain aneurysm causing a subarachnoid hemorrhage, a life-threatening condition in which a blood vessel in the brain bursts. In the emergency department, he was met by a medical team well-trained in saving lives from such neurological emergencies as stroke and aneurysm.
It was the start of a long, difficult experience, but Demachy was already on the road to recovery. Providence Little Company of Mary Torrance is considered the destination hospital in the South Bay for neurological emergencies.
Providence Little Company of Mary

Joint Commission Gold Seal of Approval
For nearly a decade, Providence Little Company of Mary has been certified as an Advanced Primary Stroke Center. The high standards set by the staff have earned the hospital The Joint Commission’s Gold Seal of Approval, and it is now the only hospital in the South Bay to carry the distinction of Comprehensive Stroke Certification by The Joint Commission. The hospital is also a recipient of the American Heart Association/American Stroke Association’s Gold Plus Achievement Award and was the first in Los Angeles County to receive an EMS designation as a Comprehensive Stroke Receiving Center.
Subarachnoid Hemorrhage Treatment
“Between 15 and 20% of patients with a subarachnoid hemorrhage like his die before they even get to the hospital,” says vascular and interventional neurologist Jason Tarpley, MD, PhD, director of the Stroke & Neurovascular Center at Pacific Neuroscience Institute—an affiliate of Providence Little Company of Mary Medical Centers San Pedro and Torrance. “Luckily, he got to us early and we made the diagnosis in the emergency department and treated him within an hour. The first priority is to fix the aneurysm as soon as you can do so safely. If it re-ruptures, or if you get a second rupture, the mortality rate is nearly 100%. So you want to get it fixed as soon as you can.”
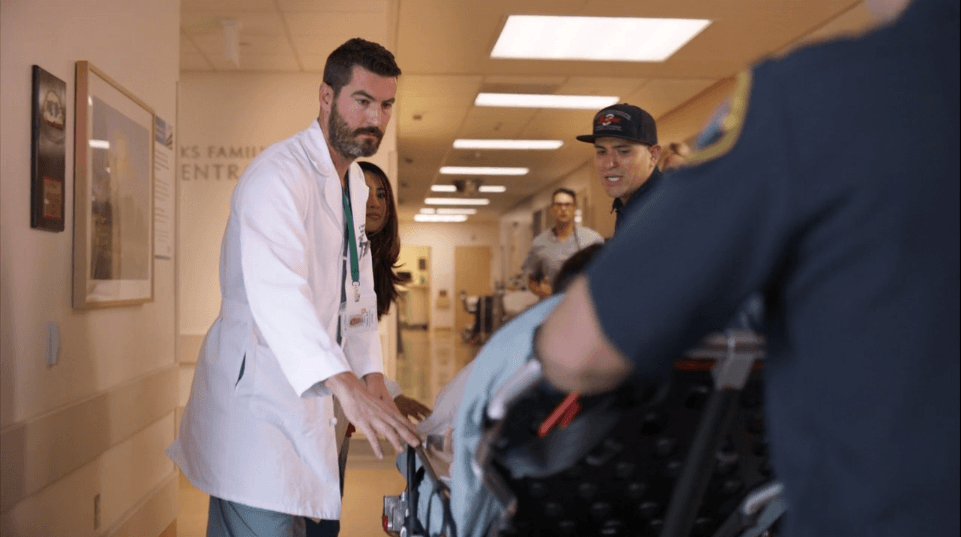
In Demachy’s case, care began when the Manhattan Beach paramedics brought him to the right hospital. The emergency room physician quickly ordered a “code stroke” and a protocol was set into motion. A brain scan showed Demachy had an aneurysm, and a multidisciplinary team converged that included Dr. Tarpley, neurosurgeon Jean-Philippe Langevin, MD, of Pacific Neuroscience Institute, and vascular neurologist Yih-Lin Nien, MD, to create a treatment plan.
Minimally Invasive Coiling
“After Dr. Langevin and I reviewed the case, we decided together that minimally invasive endovascular coiling of Charles’s aneurysm was the best treatment, and on the night of his admission I performed the coiling procedure,” Dr. Tarpley says. The minimally invasive procedure involved making an incision in the thigh and threading a telescoping catheter through the artery of the leg into the arteries of the brain, guided by imaging and a special dye. A series of smaller and smaller catheters were deployed until Dr. Tarpley placed tiny platinum coils into the aneurysm to prompt a clot to form and stop the blood flow.
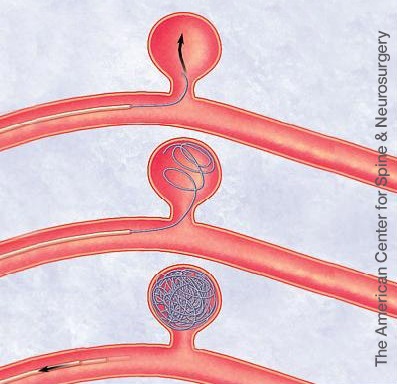
“It’s a minimally invasive option, which is usually the best way to go,” he says of the procedure. “The tiny catheter goes into the aneurysm. You fill it full of tiny platinum coils, which are like strands of platinum that ball up like a ball of yarn to plug the aneurysm. It’s a pretty amazing procedure.”
“Everything happened really fast,” says Demachy. “I remember Dr. Tarpley telling me, we have to stop the bleeding.” The coiling procedure is among the newer options for treating hemorrhagic stroke that can be offered at centers like Providence Little Company of Mary due to its top-rated stroke program.
“These are complex patients which require a lot of skill and practice,” Dr. Tarpley says. “As a comprehensive stroke center, PLCMMC is the highest volume thrombectomy center in Los Angeles, so our staff have a lot of experience.” The aneurysm was quickly secured, and then Demachy had a two-week fight in the hospital ahead of him, Tarpley says.
“The hemorrhage from aneurysm rupture causes a fascinating host of potential physiological problems that need to be handled in a multidisciplinary fashion at a comprehensive stroke center like ours,” Dr. Tarpley explains. “Charles’s subarachnoid hemorrhage caused buildup of fluid in the brain—which is common in his condition—that required Dr. Langevin to place a drain in his brain and required exquisite neurocritical care by Dr. Caganap.”
The Road to Recovery from a Ruptured Brain Aneurysm
Demachy spent two weeks in the hospital’s specialized neurocritical care unit, and was attended to by Scott Caganap, MD, a neurointensivist at Providence Little Company of Mary Torrance.
“The other critical aspect of caring for subarachnoid hemorrhage patients is neurocritical care,” Dr. Tarpley says. “Dr. Caganap monitors the patient every single day for any physiological changes so we can address issues quickly when the patient gets into trouble. Dr. Caganap managed to get Charles through fluid buildup on the brain and clots in the legs and lungs, which are all common complications of this disease process.”

“I did have a lot of complications, but I didn’t get discouraged,” Demachy says. “It was my first time at Providence Little Company of Mary Medical Center. The care was great from the beginning to the end.” He still battles occasional dizziness, but he is back to work at the Demachy family’s nursery. He can drive his car and enjoy walks on the beach with wife, Virginia.
“Subarachnoid hemorrhage can throw a lot of different punches at you,” Dr. Tarpley says. “But as a comprehensive stroke center with great neurology, neurointerventional surgery, neurocritical care and neurosurgery, we know what punches to expect and how to fight back.”
About Dr. Jean-Philippe Langevin
Dr. Jean-Philippe Langevin, is a board-certified and fellowship-trained neurosurgeon specializing in the surgical treatment of movement disorders, epilepsy and psychiatric conditions. He is Director of the Restorative Neurosurgery and Deep Brain Stimulation at the Pacific Movement Disorders Center, Providence Saint John’s Health Center and Providence Little Company of Mary Medical Center Torrance. As Director of Neuro-Spine Surgery at the Spine Institute at Little Company of Mary, he treats back issues caused by tumors, back pain, or other trauma. A multiple Super Doctor Award recipient, he has extensive experience using leading edge neurosurgical modalities to treat a wide range of conditions.
Written by Shari Roan | Photographed by Kristin Anderson
Adapted from original article in Fall 2020 issue of In Good Company, Magazine of Little Company of Mary Medical Center Torrance
Useful links
Last updated: February 16th, 2022