

The Evolution of Awake Brain Surgery
by Zara Jethani
Canst thou not minister to a mind diseased,
Pluck from the memory a rooted sorrow,
Raze out the written troubles of the brain
And with some sweet oblivious antidote
Cleanse the stuffed bosom of that perilous stuff
Which weighs upon the heart?
– Shakespeare, Macbeth, Act 5, Scene 3
Awake craniotomy is a surgical technique performed in patients with brain tumors in or near critical brain areas such as motor or speech cortex, called the eloquent cortex. This technique is most frequently used in the removal of brain tumors such as gliomas and metastatic brain tumors. During this kind of surgery, patients receive standard “asleep-awake-asleep” anesthesia, where they are sedated for the first part of the procedure. The neurosurgeon makes a small aperture in the patient’s skull and at the critical phase of tumor removal, the patient is gently awakened and the brain areas around the tumor are electrically stimulated.
A doctor keeps the patient engaged during this time by asking them to read or answer simple questions while probing the exposed brain tissue with a mild current. If the stimulation prevents or causes hesitation in the patient’s performance, or the patient experiences confusion, that area is left alone. The patient’s reactions are assessed using a neuro-monitoring technique called a functional MRI (fMRI) to determine whether it is safe to remove all or only part of the tumor. The patient goes back under sedation and the surgery is completed.
Our truest life is when we are in dreams awake.
-Henry David Thoreau
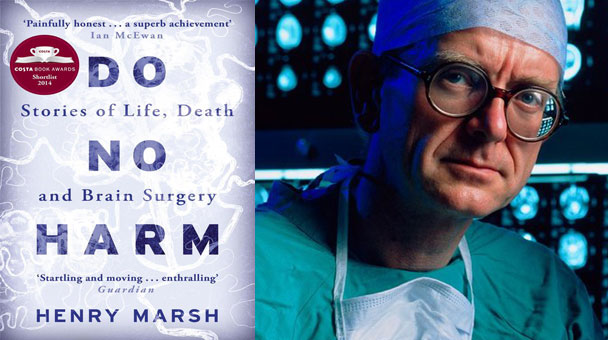
The early principles of awake craniotomy were established more than 50 years ago and were originally used in treating epilepsy. British neurosurgeon, Dr. Henry Marsh, is one of modern awake crainiotomy’s pioneers and author of the widely acclaimed autobiography, Do No Harm. He rarely practices in England now and a documentary, The English Surgeon, follows his work in the Ukraine where he has been operating since 1992. A lyrical and graphic article in the NYTimes magazine details a reporter’s experience meeting him and witnessing surgeries in progress in Albania.
Recently, Time Magazine reported the experience of awake brain surgery from one patient’s point of view during her procedure. A video documents 24 year old Brittany Capone, who had a brain tumor that was very close to the area of her brain controlling speech and comprehension. The tumor was successfully removed and she was back to work within a couple of months.
There have been some uplifting stories of musicians who have been asked to perform while in surgery to ensure that their playing ability remained unharmed.

In October 2015, 27 year old jazz musician, Carlos Aguilera, was asked to read some music and play his alto saxophone during a long surgery to remove a brain tumor in Malaga, Spain. It was a noteworthy event as this was the first time that a patient played an instrument during awake brain surgery in Spain. Aguilera has recovered fully and is back to playing in an orchestra.

And in June 2014, a Slovenian opera singer, Ambroz Bajec-Lapajne, who was diagnosed with Glioblastoma multiforme (GMB), sang excepts from Schubert’s Gute Nacht during his awake craniotomy in a Dutch clinic to remove his brain tumor. It has been over a year since his surgery, and he reports that he is doing well and has experienced no ill effects.
Awake craniotomies also help patients with essential tremors, a nervous system disorder that causes certain body parts to shake. Deep brain stimulation (DBS) for patients with these kinds of movement disorders works by using electrodes to regulate abnormal brain impulses and normalize involuntary movement. Minnesota Orchestra violinist, Robert Frisch, experienced significant improvement in his condition after receiving such treatment.
In music one must think with the heart and feel with the brain.
-George Szell (Hungarian Composer)
An unusual and novel technique called hypnosedation, was used during awake craniotomy by Dr. Ilyess Zemmoura of Centre Hospitalier Universitaire de Tours, France in patients with low grade glioma types of brain cancer. The patient is hypnotized by a medical professional and stays awake throughout the entire procedure in a state of hypnosis. The study results were mixed and they noted that there is no measurable difference in the surgical outcome. The clinical article was published in the January 2016 issue of Neurosurgery.
In the past few years we have seen the successful use of this awake craniotomy surgery increase due to advances in brain mapping techniques, sophisticated anesthetics precise monitoring of patient response and favorable results. Along with neurosurgical knowledge, experience and skill, the evolution of technology continues to help shape the advancement of surgery and medicine.
Arise! Awake! and stop not until the goal is reached.
– Swami Vivekananda
About the Author

Zara Jethani
Zara is the marketing director at Pacific Neuroscience Institute. Her background is in molecular genetics research and healthcare marketing. In addition, she is a graphic designer with more than 20 years experience in the healthcare, education and entertainment industries.
Last updated: May 5th, 2022