
Treatment for a Benign Pituitary Tumor Causing Cushing’s Disease Gives Woman Her Life Back
by Guest Author
Maple didn’t know what was happening to her. A resident of Hong Kong in her mid-20s, she suffered from frequent headaches, easy bruising, thinning hair and irregular periods. Maple blamed work-related stress and quit her job. But the symptoms persisted. Then her blood pressure started reaching alarming levels. It would take close to six years before Maple received the treatment she needed at Pacific Neuroscience Institute.
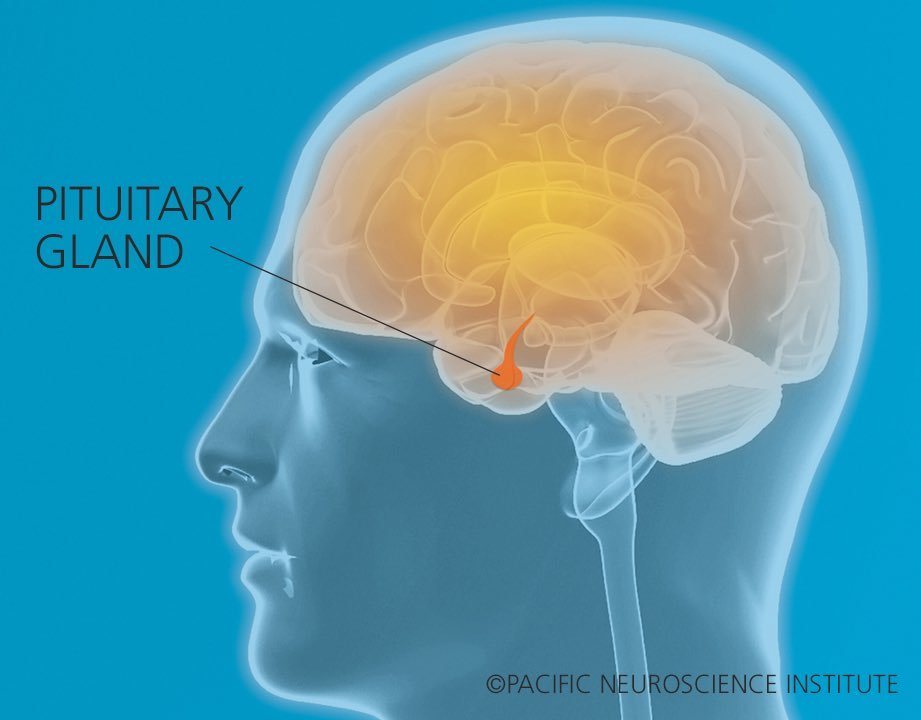
Cushing’s Disease

In Hong Kong during this time, Maple was diagnosed with Cushing’s disease. The condition is caused by a benign (non-cancerous) tumor (or adenoma) of the pituitary gland, which is located at the base of the brain. Although benign, the tumor causes excess levels of cortisol, the body’s stress hormone, which leads to a cascade of other problems. Maple underwent surgery in Hong Kong to remove the tumor, but some of the tumor remained and her symptoms persisted. Her doctors suggested a second operation to remove the entire gland.
Uncomfortable with this choice, Maple searched medical journals and websites. She discovered Pacific Neuroscience Institute and its Pituitary Disorders Center of Excellence. She learned that PNI director and neurosurgeon Daniel Kelly, MD, had extensive experience treating patients with pituitary tumors.
With Cushing’s disease, “It’s almost as if the body’s been hijacked by this tiny little tumor and it transforms the person into someone else,” says, Dr. Kelly, who notes the condition can cause weight gain, hypertension, diabetes and neuropsychological issues. “When the surgery is successful, patients get their lives and their bodies back.”
A Challenging Surgery; A Dramatic Response
At PNI, Maple received care from a multidisciplinary team that included Dr. Kelly, Ear Nose and Throat surgeon and PNI co-founder Chester F. Griffiths, MD, and specialists in endocrinology and neuroradiology.
Her tumor had grown into an area of the skull base called the cavernous sinus, which is on either side of the pituitary gland and can be difficult to reach. Removal of pituitary adenomas in this area can be risky given the proximity to cranial nerves and the carotid artery. However, thanks to their skill in endoscopic endonasal pituitary surgery, Drs. Kelly and Griffiths successfully removed the tumor and avoided injuring these sensitive structures nearby.
Endoscopic endonasal surgery uses specialized instruments, including a camera (surgical telescope), that reach the tumor via the nasal passages and sphenoid air sinus. The technique is the preferred approach for virtually all pituitary adenomas and many other midline tumors of the skull base that grow in and around the pituitary gland. It avoids disturbing the brain itself and eliminates the need for incisions.

L-R: Dr. Chester Griffiths, Amy Eisenberg NP, Maple, Dr. Daniel Kelly, & Dr. Jai Thakkur
“My life changed a lot after surgery,” says Maple. “A week later, I was able to stop taking all my blood pressure medicines. I didn’t feel the headache and swollen feeling in my head anymore. Ten days after my surgery I had lost seven pounds.”
Maple’s procedure took place in January of 2020 and she continues to see Dr. Kelly and endocrinologist Pejman Cohan, MD, for follow-up. “We continue to monitor Maple’s cortisol level to make sure it returns to normal,” says Dr. Cohan. “It takes time for the pituitary gland to fully recover after successful surgery for Cushing’s disease. And Maple will require life-long monitoring to make sure the Cushing’s doesn’t recur. I’m optimistic about her prognosis.” On a recent visit in May of this year – about 16 months post-surgery – Maple had shed almost 40 pounds, resumed her menstrual periods and had nearly normal cortisol levels.
Experience Counts
PNI has a long track record with endoscopic endonasal pituitary surgery, treating over 1000 patients since 2007 for pituitary adenomas and other related conditions. The Pituitary Disorders Center includes the disciplines of neurosurgery, ENT, neuro-ophthalmology, endocrinology, radiation oncology, neuro-oncology and neuropathology. Team members regularly teach the technique, present at national and international conferences and publish in peer-reviewed medical journals. “As a result of our expertise and reputation, we see many patients from out of state and outside the country,” says Dr. Kelly.
“Pituitary surgery is a very subspecialized niche of neurosurgery,” he adds. “Data suggests that volume matters, meaning the more you do, the better the outcomes. Particularly for a complex condition like Cushing’s disease, patients are generally best treated at a Center of Excellence where they have the expertise and experience to handle tough cases. Twenty percent of our pituitary cases are re-dos, where the patient had a prior surgery elsewhere.”
That was the key to success for Maple, who marvels at her transformation. “Sometimes I can’t believe it’s true because I struggled for so long,” she says. “I think it’s a miracle.”
About Dr. Daniel Kelly
Dr. Daniel Kelly, a board-certified neurosurgeon, is the Director and one of the founders of the Pacific Neuroscience Institute, Director of the Pacific Brain Tumor Center and Pacific Pituitary Disorders Center, and is Professor of Neurosurgery at Saint John’s Cancer Institute at Providence Saint John’s Health Center. Considered to be one of the top neurosurgeons in the US, he is a multiple recipient of the Patients’ Choice Award, and has been awarded the Southern California Super Doctors distinction 15 years in a row.
About Dr. Chester Griffiths

Dr. Chester Griffiths, is board certified in Otolaryngology, Head and Neck Surgery and Facial Plastic and Reconstructive Surgery. He has an extensive 30-year experience in endoscopic endonasal sinus surgery for skull base tumors and pituitary tumors, sinonasal cancers including mucosal melanomas, and in the treatment of facial and nasal trauma, cosmetic deformities, sinus infections, and disorders of smell and taste. His practice also includes treatment of sleep apnea, snoring, difficulty breathing, disorders of the larynx, thyroid tumors and other head and neck cancers with an emphasis on viral HPV related cancers.
Written by Nancy Steiner
Nancy Sokoler Steiner is a freelance writer in Los Angeles and a previous contributor to PNI publications.
Last updated: September 10th, 2024
