

7 Everyday Questions about Cervical Dystonia
by Zara Jethani
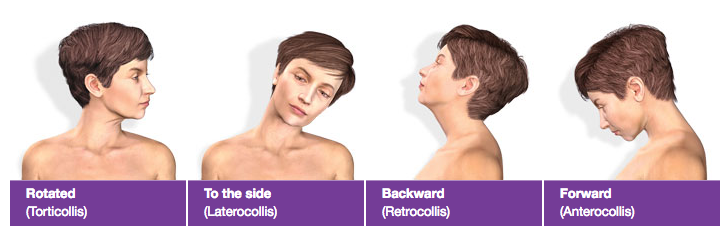
Cervical Dystonia is a painful condition that affects the neck and causes the head to tilt to one side, or causes the head to tremble. People often think that this is due to muscular issues but actually cervical dystonia is a neurological dysfunction caused by misfiring nerves.
As September is dystonia awareness month, we caught up with Dr. Melita Petrossian, Director of the Pacific Movement Disorders Center at Pacific Neuroscience Institute, to find out answers to some everyday questions that patients ask about cervical dystonia.
1. Are dystonia, cervical dystonia and spastic torticollis the same thing?
Dystonia is the term for abnormal posture or position of the muscles. It can be generalized (affecting the whole body) or focal (affecting one body part). When it affects the neck (and shoulders) it is called cervical dystonia because the word cervical means related to the neck (it has nothing to do with the female body part). Spastic torticollis and spasmodic torticollis are older synonyms for cervical dystonia.
2. I’m embarrassed about my head tilt/head tremble. What should I do?
First off, make sure you are seen by a neurologist for a proper diagnosis. Unfortunately, cervical dystonia is very commonly misdiagnosed and patients may see five providers before getting a proper diagnosis.
Typically treatment is effective for the head tilt and tremor, but for patients who still have symptoms, there are a few day to day approaches that can help. One is called a sensory trick – a light touch to the chin, or back of the head, temporarily reduces the dystonia. This is not meant to be a rough forced movement, just a sensory reminder to alleviate the symptoms for a moment.
Many patients find sitting in a high-backed chair more comfortable than a chair without neck support.
In terms of social embarrassment, it really depends on the situation whether patients wish to divulge the cause of the head shaking or not. A simple declaration that they’re not nodding yes or no, but rather dealing with a tremor, may be all that’s necessary.
3. What’s the difference between cervical dystonia and a neck sprain?
Neck sprains are very common and may cause a temporary abnormal posture with associated pain. Massage and stretching will help for these and they typically resolve in a few days or weeks. Cervical dystonia is usually lifelong, even though it does not begin until middle age (commonly). Cervical dystonia comes from the brain sending abnormal signals to the muscles, resulting in an incorrect set point. Neck sprains, sometimes called cervical sprain or muscle sprain, come from the muscles.
4. Does physical therapy help treat cervical dystonia?

It depends on the familiarity of the therapist with the diagnosis. Many patients with cervical dystonia may experience lack of improvement or sometimes even in some cases worsening of their dystonia if they are being treated as if they had muscle spasm or degenerative disc disease.
However, physical therapists with specialty in neurological disorders (neuro-PTs) are well versed in cervical dystonia and can definitely benefit, especially when combined with botulinum toxin injections. Neuro-PT has more focus on re-educating the neurological system, using modalities such as sensory reintegration, mirror therapy, and even in some causes virtual reality to correct the abnormal set-point caused by the brain. There is evidence that PT can help the effects of botulinum toxin last longer.
5. What cervical dystonia treatment do you recommend?
Usually just botulinum toxin injection is enough to manage the symptoms of cervical dystonia, including pain, tightness, tremor, and abnormal position of the head and shoulders, sometimes in conjunction with a skilled neuro-PT as above.

Botulinum toxin injection works by reducing the communication between nerves and targeted muscles. This weakens the overactive muscle. In certain cases the injections need to be adjusted. As the months or years go by, there may be different muscles involved, or different areas of the muscles are more active, or higher doses are required. Botulinum toxin injections are typically done every three months.
For cases where the combination of injections and physical therapy are insufficient in managing the dystonia, we can consider the use of oral medications such as trihexphyenidyl (Artane), baclofen, or clonazepam (Klonopin). These can relax muscles but can also cause side effects such as weakness, fogginess, dry mouth, or constipation.
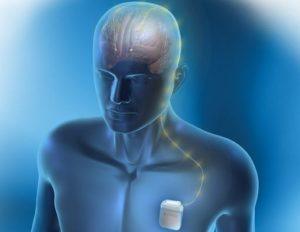
In cases where neither injections nor medications have helped, deep brain stimulation (DBS) surgery can be considered. There is a long history of success with DBS for cervical (and other causes) of dystonia, but not everyone responds to the same extent.
DBS surgery involves the placement of electrical leads in specific targets in the brain, linked to a battery / pulse generator in the chest below the collar bone. This is similar to a pacemaker, except it is controlling certain brain signals rather than the heart.
6. Is cervical dystonia rare?
Not particularly. It affects about 60,000 people in the United States but it is quite likely that this number is in reality much higher, given the number of patients who go undiagnosed.
7. Are there cervical dystonia support groups that I can go to?
Yes, there is a foundation called the NSTA (National Spasmodic Torticollis Association) which has support groups in Long Beach and other areas in Southern California. Also there is a dystonia support group in Los Angeles, but it is not specific to cervical dystonia. There are also facebook groups and online support systems that are convenient for those who cannot make it to an in-person meeting.
Contact Pacific Neuroscience Institute
To find out more about Deep Brain Stimulation (DBS) please contact our restorative neurosurgeon, Dr. JP Langevin at the Pacific Movement Disorders Center.
Dr. Melita Petrossian’s clinics are located at the Pacific Movement Disorders Center at Pacific Neuroscience Institute in Santa Monica and Torrance, CA. For a consultation or more information about dystonia, please call at 310-582-7433 or visit PacificMovement.org.
About Our Movement Disorders Expert

Dr. Melita Petrossian is a Harvard-trained Neurologist and Movement Disorders specialist and is the Medical Director of Pacific Movement Disorders Center at Providence Saint John’s Health Center and Providence Little Company of Mary Medical Center in Torrance. Dr. Petrossian’s clinical interests and expertise are in movement disorders such as Parkinson’s disease (PD), tremor, dystonia, gait disorders, ataxia, myoclonus, blepharospasm, hemifacial spasm, spasticity, and tics; as well as Parkinson’s-related conditions such as Dementia with Lewy Bodies, progressive supranuclear palsy, and multiple system atrophy.
Dr. Petrossian’s focus is on a multidisciplinary approach to these movement disorders, including appropriate diagnosis utilizing the latest imaging techniques such as MRI, PET and DaTscan; optimization of medical treatment; Botulinum toxin injections; and coordination with physical therapists and speech therapists. She assesses patients for deep brain stimulation surgery and creates a custom-tailored program of DBS settings. She is a member of the American Academy of Neurology and Movement Disorders Society.
Read Other Dystonia Articles from Pacific Neuroscience Institute
About the Author

Zara Jethani
Zara is the marketing director at Pacific Neuroscience Institute. Her background is in molecular genetics research and healthcare marketing. In addition, she is a graphic designer with more than 20 years experience in the healthcare, education and entertainment industries.
Last updated: December 16th, 2022


