Reconnecting After Hearing Loss
by Guest Author
The team at the Adult and Pediatric Cochlear Implant Program, Dr. Courtney Voelker and Dr. Rebecca Lewis, tackled hearing loss and restored Father Timothy McGowan’s hearing so he could get back to the work he loves.
When Father Timothy McGowan realized that with his progressive hearing loss he could no longer hear what parishioners were telling him during confession, he thought to himself, “Well, someone’s prayers are being answered, but not mine!” The 72-year-old priest, who had long grappled with fluctuating hearing loss caused by an autoimmune disorder, finally had to admit to himself that even with his hearing aids, he couldn’t hear well enough to perform his spiritual duties at the Church of the Visitation in Westchester.
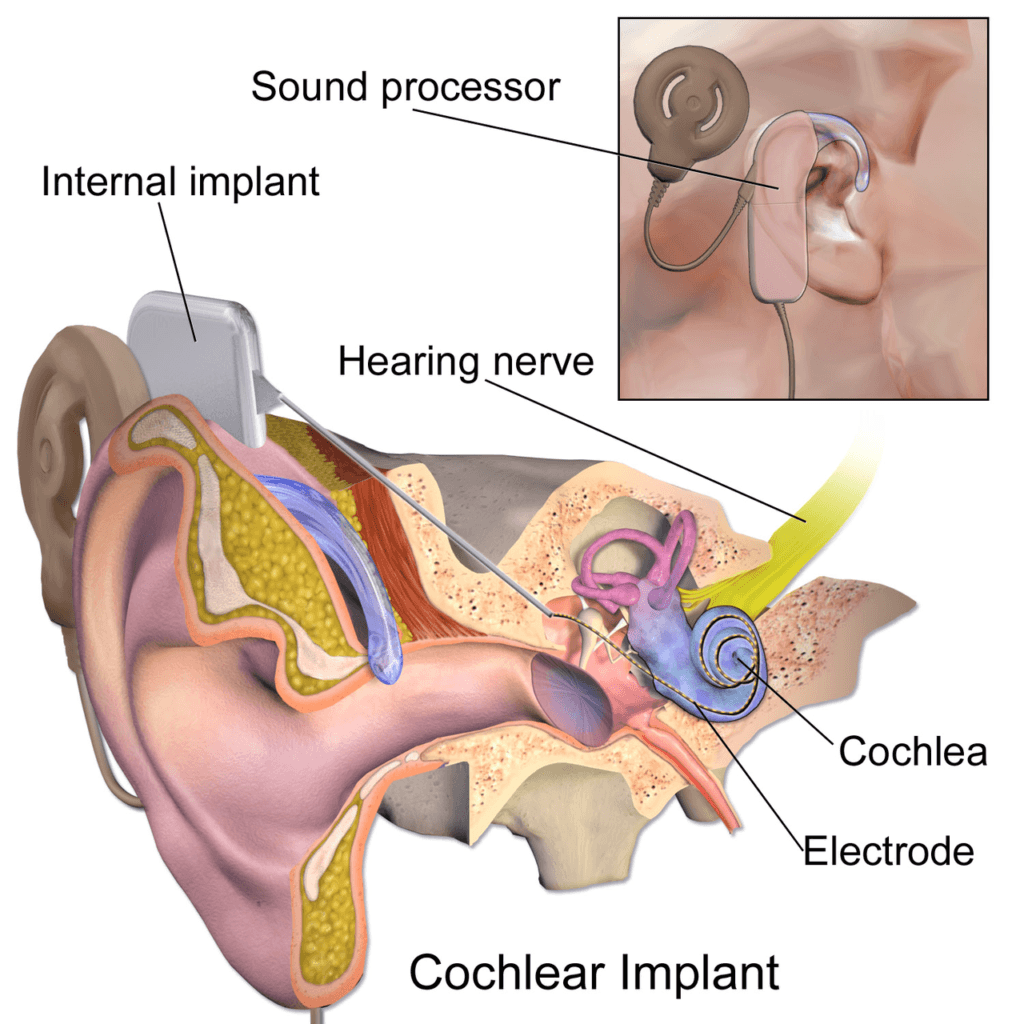
Making things more difficult, Father Tim’s hearing loss hit its worst point during the pandemic. “It was very isolating,” he recalls. “I couldn’t talk on the phone. I couldn’t listen to music or watch TV.” The type of hearing loss he experienced is known as sensorineural hearing loss, and it is by far the most common. It affects the inner ear, where the snail shell–shaped cochlea translates sound waves into electrical signals that travel via the auditory nerve to the brain.
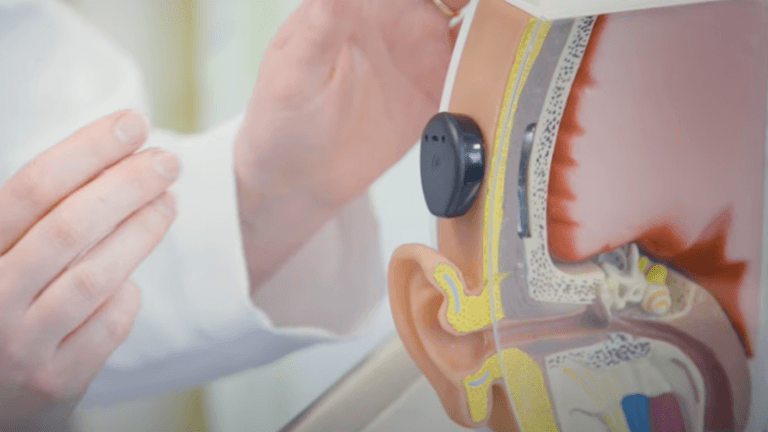
Fortunately, Father Tim’s severe hearing loss was correctible with cochlear implants. Cochlear implants are small devices that contain two parts: an external processor that picks up sound and an internal receiver attached to a wire that’s threaded into the cochlea. The systems are Bluetooth-compatible, which means the wearer can receive phone calls, TV audio and external mic sound directly to the receiver. Since they were first approved by the Food and Drug Administration in the 1980s, cochlear implants have become increasingly miniaturized.
Meeting the Cochlear Implant Team
Neurotologist Courtney Voelker, MD, PhD, and audiologist Rebecca Lewis, AuD, who make up the team at the Pacific Neuroscience Institute®’s Adult and Pediatric Cochlear Implant Program at Providence Saint John’s Health Center, were the ones who helped Father Tim recover his vocation and more, including riding his motorcycle safely again and traveling abroad for the first time in years.
After establishing the program, Dr. Voelker performed Providence Saint John’s first cochlear implant in 2022. Dr. Voelker and Dr. Lewis are strong advocates for the procedure in people with significant hearing loss. In infants, the development of language and speech hinges on early exposure to sound, and in older adults, staying connected to the world through hearing staves off—or even can reverse—dementia. “We are learning that hearing loss is the number one predictor of cognitive decline. As little as six months of wearing a hearing aid or implant can reverse it,” says Dr. Voelker.
“Hearing loss is an invisible disease,” adds Dr. Lewis. “It’s isolating; it’s depressing. People start to retreat from the world. Treating their hearing loss helps them reengage.” According to the National Institute on Deafness and Other Communication Disorders, 25% of people aged 65 to 74 experience disabling hearing loss. By age 75, a full 50% of people have it.
Dr. Voelker explains that the two- to three-hour implant procedure is done under general anesthesia and that patients go home the same day. It involves making an incision behind the ear for the receiver and drilling a small hole in the mastoid bone for the wire that’s threaded into the cochlea. After a week or more of healing, the patient returns to have the implant activated.
At that point, the patient works with Dr. Lewis to fine-tune the device and acclimate to it. “It’s a process,” she explains. “It’s not a quick fix.” That’s because the brain has to learn how to interpret this new form of electrical impulse that’s coming through the auditory nerve. Some people understand speech immediately, while others hear only indistinct sounds the first day. “I love seeing people for the three-week and three-month visits, because we see such dramatic progress,” says Dr. Lewis.
Hearing Restored and Back To Life
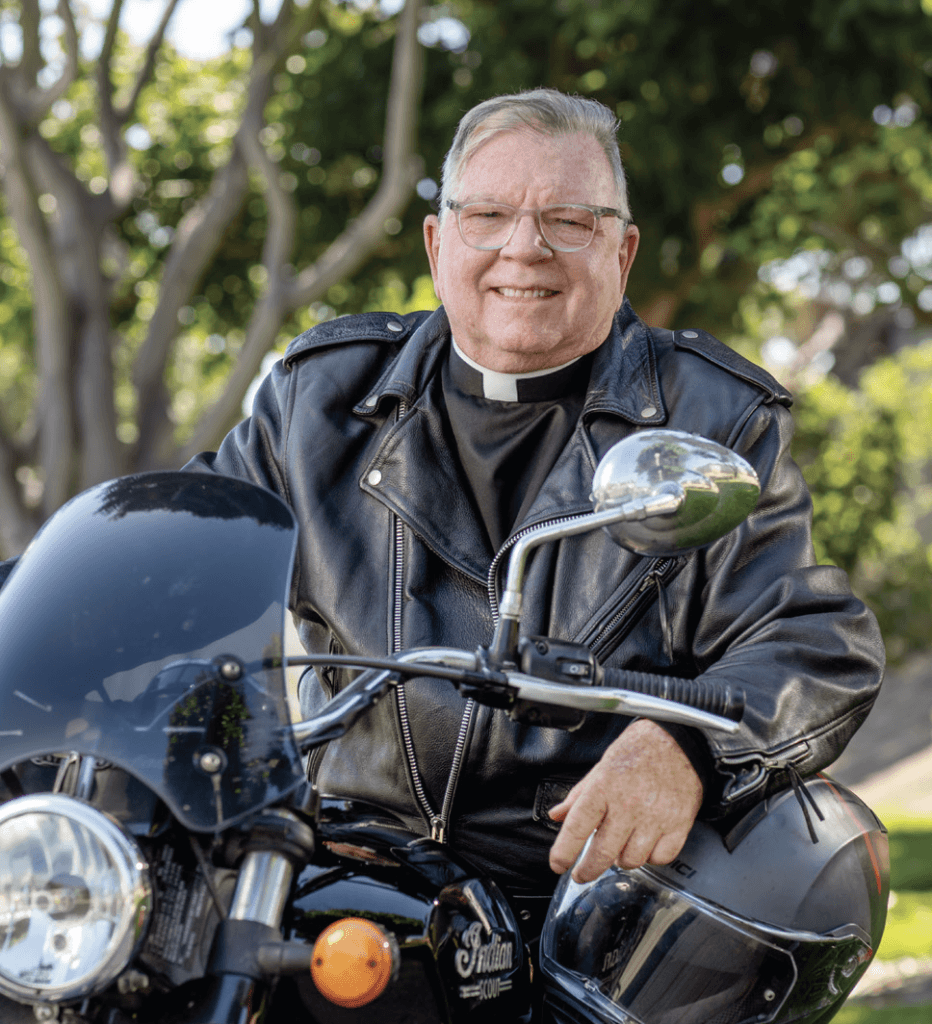
Father Tim got his first implant in his right ear in November 2022 and his second in the left in May 2023, and he remembers being able to understand speech immediately even with the first one. “I’m so grateful that I don’t feel any hesitation about being able to do my work now,” he says. He has returned to serving at Visitation Parish and as chaplain at St. Bernard High School, work he had reluctantly given up.
“He really lit up when he finally could communicate with more confidence,” Dr. Lewis recalls.
Learn more about Pacific Neuroscience Institute’s cochlear implant program.
Adapted from the original article in Health Matters Summer issue 2024.
About Dr. Courtney Voelker
Courtney Voekler, MD, PhD (DPhil Oxon.), is a Rhodes Scholar and board certified neurotologist and cochlear implant surgeon who takes care of adult and pediatric patients seeing a wide range of inner ear and skull base conditions. She developed PNI’s enhanced treatment protocol for the treatment of acoustic neuromas. For qualified patients who suffer hearing loss before or after surgery, a cochlear implant may be placed in the affected ear to restore hearing at the time of tumor removal—a unique feature offered at few institutions.
About Dr. Rebecca Lewis

Rebecca Lewis, AuD, is an audiologist and the Audiology Director of the Adult & Pediatric Cochlear Implant Program at Pacific Neuroscience Institute. She also holds the position of Adjunct Professor at Mount Saint Mary University / John Tracey Deaf and Hard of Hearing program. She has provided rehabilitative services including hearing aids, hearing protection, Osseo integrated devices, auditory brainstem implant and cochlear implant (CI) services to adults and children.
Cochlear Implant Clinic Location
11645 Wilshire Blvd., #600, Los Angeles, CA 90025
310-477-5558
Useful Links
- Pacific Eye, Ear & Skull Base Center
- Cochlear Implants
- Hearing Restoration
- Brain Wellness & Lifestyle program
Last updated: October 1st, 2024