

Glioblastoma at the Time of COVID-19
by Akanksha Sharma
In February 2020, a beautiful and energetic young woman in her late 30s gave birth to her second child. In the week and months after, the world changed around her. Inside, she felt strange too – exhausted, moody, very irritable, forgetful all the time. Maybe it was the stress of a newborn baby. Of being a mother. Of motherhood during the pandemic. But then, in June of 2020 she had a seizure and was taken to the hospital where she had a scan of her brain.
When Glioblastoma Strikes
She became one of 13,000 Americans diagnosed with glioblastoma (GBM) in 2020, an aggressive brain cancer that results in the death of almost 10,000 Americans a year. Unfortunately, GBM grows quickly, often silent initially, infiltrating healthy brain tissue, until the inflammation it causes results in symptoms. These may include headaches, sudden seizures, weakness, numbness, tingling, confusion and personality changes, to list just a few. Regardless of how it appears, the diagnosis of GBM inevitably changes the life of the patient and their loved ones.
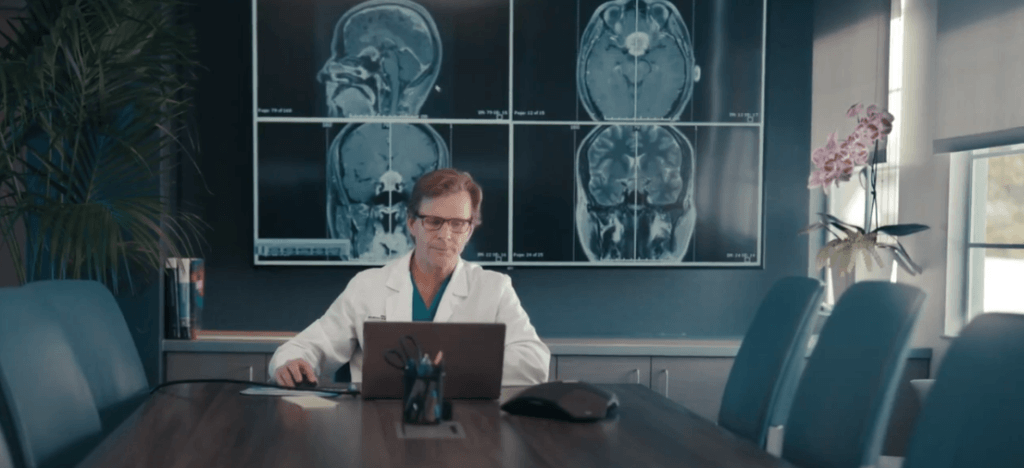
As a neuro-oncologist specializing in palliative care at the Brain Tumor Center at Pacific Neuroscience Institute, I am mindful that after that first conversation in our offices, patients are wrapped up in a storm of emotion – fear, anger, shock – all of it enveloping and overwhelming them. Web search engines provide a series of difficult facts – the five-year survival rate for GBM is only around 10%, the average length of survival for GBM patients is 16-22 months, even in 2021, with treatment.
The Value of Time
The value of each day, week and month, every special occasion, becomes truly evident when time becomes a limited and precious resource. While our currently available treatments for GBM add only a relatively limited amount of time to a patient’s life, that time is not trivial. Rather, it is valuable and worthwhile. Sometimes it means getting to a wedding, a birth, a graduation. Sometimes it means making sure a loving legacy is set up for those left behind. Sometimes it means more time to build memories and share the simple moments. I have learned from my patients and their families the importance of each moment in my own life, with my own loved ones.
The Impact of COVID-19
When time is so precious, we try to spend every single moment with the people who are close or doing the things we love. This all changed in March 2020, when the COVID-19 pandemic lockdown changed the world. Suddenly, our patients with GBM and other cancers and tumors became increasingly isolated, limited in their ability to go outdoors, to travel, unable to visit with family and friends, see children and grandchildren grow, hug and be hugged and held.
Hospital visitation restrictions limited the presence of family members for surgeries, hospitalizations, appointments and treatment visits. This was especially impactful for patients with GBM, where the disease can influence thinking and cognition. To alleviate the situation, we appealed to our hospital leadership and were granted special visitation privileges for hospitalized patients. We ensured that when critical, a family member could accompany a patient for a clinic visit.
Hospitalization was particularly harmful. Alone in the hospital, our patients were at risk for becoming hopeless, dejected and distraught. Often, they became delirious – a state of confusion that is brought on in new places without familiar faces, especially in patients who are neurologically fragile – which made their recovery even more challenging. The longer they stayed in the hospital, the more isolated they became, the more at risk they became for other complications and infections, especially becoming at risk for COVID-19.
Providing Virtual Care
Around the country and the world, the neuro-oncology world focused on addressing the impact of the pandemic on our patients as much as possible – the same was true for our group here at PNI. For patients getting surgical interventions for their tumors, post-operative stays were kept as short as safe and feasible. For the rest of our patient panel, we made sure they stayed healthy and safe, and that we addressed concerns and symptoms quickly and remotely, keeping them out of the ER.
Patients with GBM can have any number of complications during their journey. The brain controls our thinking, memory, personality, our senses, our ability to move and feel and empty our bladder. Aside from this, GBM is an aggressive cancer, and any patient with cancer is at risk for a number of issues – clotting, infection, bleeding, and so on. Our patients may experience a number of symptoms that warrant evaluation and management urgently. Yet, during the surges of the pandemic, this was not feasible and could do more harm than good. In addition, our hospital services were exhausted and at one point there was no capacity at all.
We transitioned our care to virtual visits as much as we could, we brought in only those patients who needed infusions and treatment, and we were vigilant about messages and calls regarding changes in our patients’ conditions. Our team here at PNI focused on addressing symptoms as quickly as we could in an outpatient setting – getting patients in for an infusion of steroids or pain medications if needed, sending antibiotics outpatient to get on top of infections quickly, virtually examining a patient who was confused and arranging imaging outpatient. Anything we could do, at any time of day, to triage and ensure only those who absolutely needed admission were sent to the hospital.
Patient and Team Approach
This type of work is not possible without a team. I joined this team during the October 2020 surge and I immediately saw how incredible, selfless and hardworking the entire team – from front desk staff to radiology techs to the clinicians – remained throughout the pandemic to take care of our patients. But this would also not be possible without the incredible trust and belief our patients and their families place in us. They trusted us to know when to worry, when not to worry, trusted our advice and our recommendations, and the majority of them listened when we asked them to stay safe at home.
Getting Vaccinated

We were fortunate that we lost very few patients, if any, to COVID-19 during this pandemic across all the hospital systems the neuro-oncology team works at in the SoCal area. We gradually transitioned our efforts to ensure our patients and their families were vaccinated, showing off our own vaccine card and discussing our experience as soon as we got ours!
We know that the risk of infection and of hospitalization is much higher than any possible side effects from the vaccine – we also know what it has taken to protect our patients from infection and its sequelae. Our patients value their time with their families, at home, doing the things they love, traveling, making precious memories – and we know that vaccination against COVID-19 provides them with the protection they need so they have more of that quality time. None of our vaccinated patients have had any type of unusual reaction or side effects to the COVID-19 vaccine.
Glioblastoma Awareness
As Glioblastoma Awareness Day approaches, this year on July 21, 2021, I reflect on the work I do and all the patients who have had such an impact on my life. I reflect on the memories of the patients I have lost, but who have taught me so many important lessons during their lives. I think of the patients and loved ones who are going through their journey right now with such immense courage and hope, facing a diagnosis like GBM along with the uncertainties and challenges of a global pandemic.
I became a neuro-oncologist to be present for patients and their loved ones during this last phase of life. To help guide, provide council, and create a space to speak openly about hopes, fears, quality of life, anything that is on their minds. I am privileged to treat and care for some of the most inspiring, most incredible human beings in the entire world, and it is this sense of awe that drives me to continue this work every day.
Inspiring Patient Stories
- Frank’s Story (Video)
- Rusty’s Story (Video)
Related Links
About the Author

Akanksha Sharma
Akanksha Sharma, MD, is board certified in neurology, neuro-oncology and palliative medicine. She is experienced in the treatment of primary/metastatic brain tumors, neurological complications of cancer, and disease-related burden and symptoms. Her clinical and research interests lie in helping patients maximize their time and quality of life. She aims to align treatment with patient goals and to provide holistic care that includes careful symptom assessment and management, as well as support for the patient’s loved ones.
Last updated: July 2nd, 2021