

Understanding Normal Pressure Hydrocephalus Treatment: A Guide
by Zara Jethani
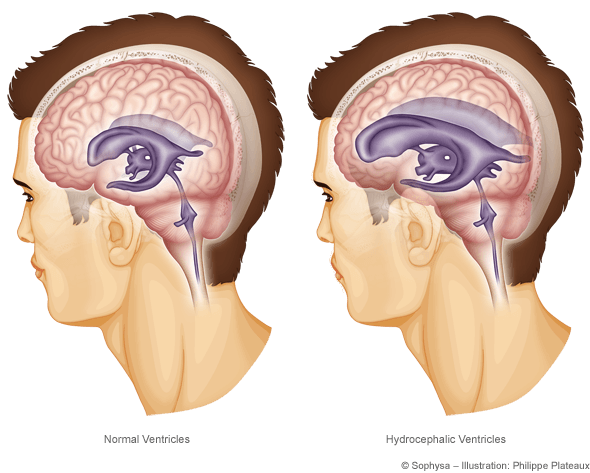
Hydrocephalus is a condition of excess fluid on the brain. The brain and spinal cord are normally bathed by cerebrospinal fluid (CSF) which gives the brain buoyancy and acts as a shock-absorber, and is produced in fluid-filled structures called ventricles. CSF cycles through the system but If there is blockage along the drainage pathway or if the fluid cannot be absorbed back into the blood, then the fluid backs-up into the ventricles, causing enlargement known as hydrocephalus.
What is Normal Pressure Hydrocephalus?
Normal pressure hydrocephalus (NPH) is a neurological disorder that predominantly affects adults, particularly those over the age of 60. This condition is characterized by an abnormal accumulation of cerebrospinal fluid (CSF) in the brain’s ventricles, leading to increased pressure that can damage brain tissues. Despite the name, “normal pressure” refers to the fact that CSF pressure often remains within normal ranges when measured, yet the fluid buildup still causes significant issues.
Symptoms of Normal Pressure Hydrocephalus
The symptoms of normal pressure hydrocephalus can often be mistaken for other conditions like dementia, Alzheimer’s disease or Parkinson’s disease, which can make diagnosis challenging. The hallmark symptoms of NPH include:
- Gait Disturbances: One of the earliest and most noticeable symptoms of NPH is difficulty walking. Patients may exhibit a shuffling gait, where steps become shorter and more difficult to initiate.
- Cognitive Decline: NPH can cause problems with memory, attention, and decision-making, often resembling dementia. However, unlike Alzheimer’s, the cognitive symptoms of NPH can be reversible if treated early.
- Urinary Incontinence: Incontinence or frequent urination can also occur as the condition progresses. This symptom, combined with the others, often leads to a misdiagnosis of other age-related conditions.
How Quickly Does Normal Pressure Hydrocephalus Progress?
Normal pressure hydrocephalus (NPH) typically progresses slowly, but the rate can vary among individuals. NPH is a condition where excess cerebrospinal fluid accumulates in the brain’s ventricles, causing pressure without significant increases in intracranial pressure. Symptoms often develop gradually over months or even years, making early detection challenging. The symptoms of normal pressure hydrocephalus may worsen over time if left untreated. However, since NPH symptoms can resemble other neurological disorders, such as Alzheimer’s or Parkinson’s disease, it’s important to receive an accurate diagnosis as early as possible.
Diagnosing Normal Pressure Hydrocephalus
Accurate diagnosis of normal pressure hydrocephalus is important for effective treatment. Diagnosis typically involves a combination of neurological exams, brain imaging (such as MRI or CT scans), and sometimes a lumbar puncture (spinal tap) to measure CSF pressure. The characteristic ventriculomegaly (enlarged ventricles) seen on imaging, combined with the clinical symptoms, helps physicians determine the presence of NPH.
“We have a formalized protocol for diagnosis, work-up, treatment and post-surgical evaluation, including metrics, to monitor the progress of each patient,” says Garni Barkhoudarian, MD, director of the Pacific Adult Hydrocephalus Center at Pacific Neuroscience Institute®. “For adult patients with hydricephalus due to lesions in the brain, such as colloid cysts or tumors, or neuroendoscopic techniques allow for appropriate and minimally invasive methods to surgically treat these patients. Finally, differentiating between NPN and non-NPH conditions is critical with regards to assessing the patient and identifying the correct diagnostic and treatment pathways for each patient.”
Treatment Options for Normal Pressure Hydrocephalus
The most common and effective treatment for normal pressure hydrocephalus is the surgical placement of a shunt system. Ventriculoperitoneal (VP) shunting involves placing a small tube, or shunt, into the brain’s ventricles to drain excess cerebrospinal fluid (CSF) into the abdominal cavity, where the body absorbs it. By relieving pressure on the brain caused by fluid buildup, this treatment can significantly improve symptoms like difficulty walking, memory loss, and urinary incontinence.
VP shunting is the most effective treatment for NPH, especially when performed early in the disease’s progression. The goal is to reduce fluid buildup and restore more normal brain function. However, like any surgery, shunt placement carries some risks, such as infection or shunt malfunction, which may require further intervention.
Before surgery, doctors typically perform a lumbar puncture or external lumbar drainage to assess how well the patient responds to CSF drainage. This step helps confirm whether shunting will improve symptoms and ensures the best possible outcome.
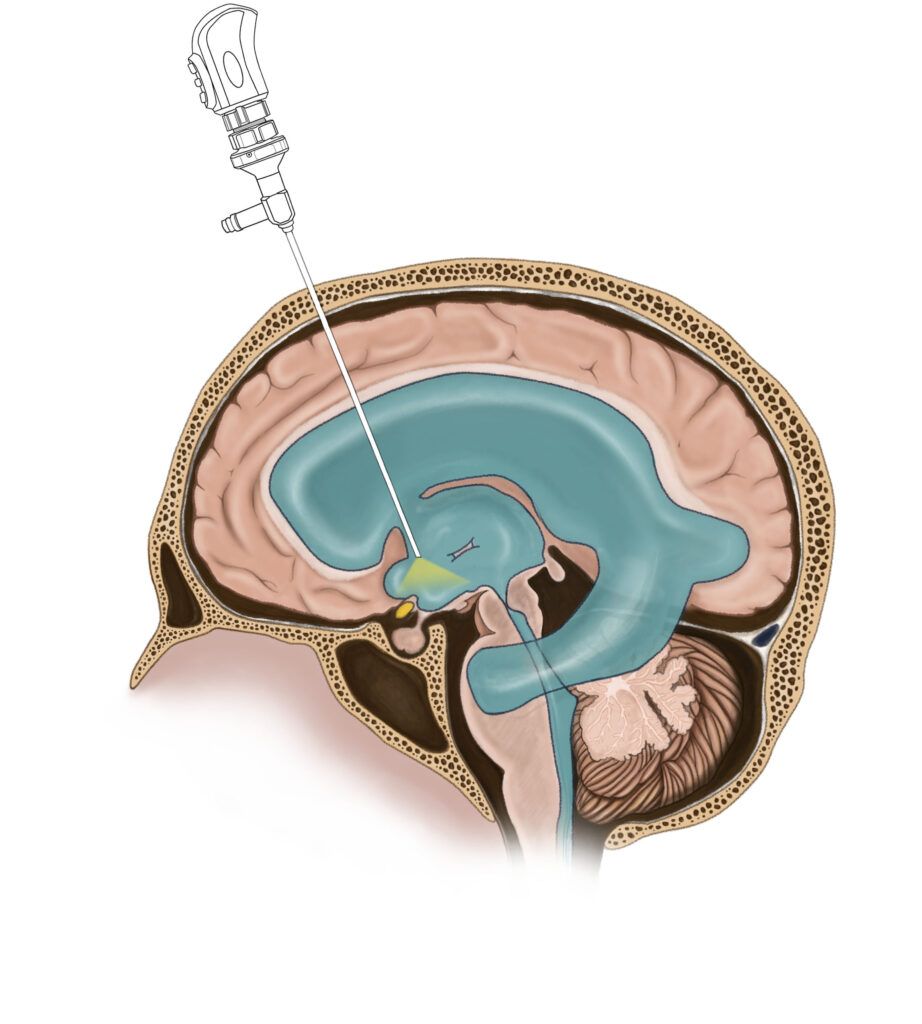
Other treatment options include endoscopic third ventriculostomy (ETV), a less common procedure that creates an opening in the third ventricle to allow fluid to bypass the obstruction. In some cases, medication or physical therapy may be recommended to manage symptoms.
Why Early Detection of Normal Pressure Hydrocephalus is Important
Early detection and treatment of normal pressure hydrocephalus are essential because they can lead to a full recovery or significant improvement in symptoms. If left untreated, NPH can lead to severe and irreversible brain damage. Therefore, if you or a loved one is experiencing symptoms of NPH, it’s essential to seek medical attention promptly.
Clinical Trials
At Pacific Neuroscience Institute®, we are participating in clinical research to improve diagnosis, management, and outcomes of NPH. The Efficacy in Idiopathic Normal Pressure Hydrocephalus (iNPH) Shunting (PENS) trial is a multi-center blinded, randomized, placebo-controlled design investigation of cerebrospinal fluid (CSF) shunt surgery to study the shunt efficacy in iNPH patients. The term idiopathic is used to describe NPH that arises spontaneously with no identifiable cause.
Normal Pressure Hydrocephalus Treatment at Pacific Neuroscience Institute
If you or someone you know is experiencing symptoms of normal pressure hydrocephalus, it’s important to consult with a specialist who understands this condition. At the Pacific Adult Hydrocephalus Center at Pacific Neuroscience Institute, our team, led by center director Garni Barkhoudarian, MD, offers expert diagnosis and treatment options tailored to each patient’s needs. Contact us today to schedule a consultation and take the first step towards recovery.
What is the long term prognosis for normal pressure hydrocephalus?
The long-term prognosis for normal pressure hydrocephalus (NPH) varies depending on factors such as how early the condition is diagnosed, how quickly treatment is initiated, and the individual’s overall health. When treated with ventriculoperitoneal (VP) shunting, many patients experience significant improvements in symptoms like walking difficulties, cognitive decline, and urinary incontinence. Early intervention for normal pressure hydrocephalus typically leads to better outcomes, especially regarding mobility and daily functioning.
However, the degree of improvement from treatment of hydrocephalus can vary. While some patients may regain nearly normal function from hydrocephalus treatment, others may have lingering symptoms, particularly if the condition was left untreated for a long time before surgery. In some cases, symptoms can recur if the shunt for NPH malfunctions or becomes blocked, requiring further medical attention.
Cognitive symptoms, such as memory issues or dementia, tend to improve less dramatically than physical symptoms, and not all patients recover fully in these areas. Regular follow-ups with your doctor are essential to monitor the shunt’s function and to manage any potential complications from NPH.
- Long-term prognosis depends on:
- Early diagnosis and treatment
- Individual response to shunting
- Managing potential shunt-related issues
How Long Do Shunts for Hydrocephalus Treatment Last in Adults?
Shunts used for normal pressure hydrocephalus (NPH) in adults typically last for several years, though the exact duration can vary depending on factors such as the patient’s condition and any complications that arise. Many shunts can function effectively for 5 to 10 years or longer. However, shunts are mechanical devices, and they are not immune to issues like blockages, infections, or over-drainage, which may require surgical revision or replacement.
Regular monitoring and follow-up care are essential to ensure the shunt continues to function properly. If problems occur, shunt malfunction symptoms—such as a return of hydrocephalus symptoms (e.g., difficulty walking, memory loss, or headaches)—should prompt immediate medical attention to determine if the shunt needs repair or replacement.
About Dr. Garni Barkhoudarian
Garni Barkhoudarian, MD, FAANS, is a board-certified, fellowship-trained neurosurgeon with a focus on skull base and minimally invasive endoscopic surgery. Dr. Barkhoudarian has particular interest and expertise in pituitary and parasellar tumors, brain tumors, skull-base tumors (including meningiomas, craniopharyngiomas, chordomas and schwannomas), intra-ventricular brain tumors, colloid cysts, trigeminal neuralgia, hemifacial spasm and other vascular compression syndromes.
Clinic Locations
2125 Arizona Ave.,
Santa Monica CA 90404
310-582-7450
501 S Buena Vista St.,
Burbank, CA 91505
818-847-6049
5215 Torrance Blvd., #300
Torrance, CA 90503
424-212-5361
Useful Links
About the Author

Zara Jethani
Zara is the marketing director at Pacific Neuroscience Institute. Her background is in molecular genetics research and healthcare marketing. In addition, she is a graphic designer with more than 20 years experience in the healthcare, education and entertainment industries.
Last updated: December 17th, 2024