

Cervical Dystonia: A Pain in the Neck
by Melita Petrossian
Content: Symptoms | Diagnosis and Treatment | A Surgical Option | Useful Resources
What is Cervical Dystonia?
Cervical dystonia, also known as spasmodic torticollis, is a neurological disorder that causes involuntary contractions or spasms of the neck muscles, leading to abnormal movements and postures of the head and neck. This condition can cause significant pain, discomfort, and disability for affected individuals.
The exact cause of cervical dystonia is not fully understood, but it is believed to involve dysfunction of the basal ganglia, a group of structures in the brain that are responsible for controlling movements. Some cases of cervical dystonia may be associated with genetic factors, while others may be triggered by trauma, infections, or exposure to certain medications or toxins.
An under-recognized cause of neck pain and muscle spasm
Many of our patients tell us that prior to being seen by us, their symptoms were dismissed by physicians or other providers. Because many movement disorders show no abnormalities on blood testing or imaging, patients are often told that there is “nothing wrong” and that they should learn to “live with it.”
This was Ella’s experience. Ella had been suffering from a tremor, which caused her head to move uncontrollably from side to side, adversely affecting her quality of life and impacting her work. She visited a number of specialists who were either unable to diagnose her symptoms, telling her to live with it, or misdiagnosing her condition and providing treatment options that were inappropriate and ineffective. Fed up, she resigned herself to a limited quality of life and social embarrassment.
Time passed and Ella needed to see a specialist for the evaluation of an unrelated headache. She was referred to Dr. Melita Petrossian, neurologist and medical director of the Pacific Movement Disorders Center who was able to reassure Ella that her headache was benign and would resolve. Then Dr. Petrossian said, “Has anyone ever told you that you have cervical dystonia and that it’s treatable?” Ella burst into tears. After 12 long and agonizing years, she finally had a medical diagnosis and a treatment plan.
Treating Dystonia with Botox
Listen to Dr. Diaz on The Think Neuro Podcast mini talk about how botox can ease can help ease the symptoms.

Cervical dystonia refers to the abnormal posture of the muscles of the neck, resulting in a twisted, turned, flexed or extended neck position. This strained positioning is brought on by abnormal signals coming from the deep parts of the brain. Because it is of neurological origin, from brain signals, it’s not the same as having a crick in one’s neck and won’t resolve with muscle massage or stretching. The word cervical in the term cervical dystonia should not be confused with the female reproductive organ, known as the cervix. The word cervical comes from the word cervix, which literally means “neck”. The female “cervix” refers to the “neck” of the uterus (womb)— if you imagine the uterus to be the head, the cervix is its neck. Cervical dystonia, then, is the medical term for neck dystonia. Both men and women can be affected.
Symptoms of Cervical Dystonia
Patients find that the abnormal positioning cannot be easily overcome. Sometimes they can improve their neck posture temporarily but often this is associated with neck pain or the sensation of straining their neck when trying to assume a normal position. Cervical dystonia can manifest as pain or discomfort. Patients often report that touching their head or face in a particular way can temporarily improve the position; this is known as a geste antagoniste or sensory trick. For example, sitting in a chair with a high back, or leaning one’s head against the wall, can temporarily reduce discomfort from abnormal positioning. Stress may worsen dystonia and relaxation techniques can help somewhat.
Cervical dystonia can often manifest for years without an accurate diagnosis, and unfortunately, patients suffer without proper treatment. In one study, it took an average of 7 years from symptom onset to diagnosis of cervical dystonia, and more than 50% of patients sought physical therapies initially, such as a chiropractic, massage, heat, or stretching.
This highlights the frequent misconception that their symptoms are due to a musculoskeletal cause of neck pain: “I must have slept wrong on my pillow”; “I pulled a muscle”; “I have a slipped disc.” Patient unfamiliarity of cervical dystonia is understandable and common, but unfortunately, it seems physician lack of recognition is an issue as well.
In the study, patients were seen by an average of 3 doctors prior to being diagnosed, but this ranged from one to nine doctors. Also, about half of patients with cervical dystonia complain of neck pain, so patients and physicians often think of the more common causes of neck pain such as musculoskeletal strain or cervical radiculopathy (pinched nerve).
Experiencing pain or symptoms that concern you?
While it is relatively uncommon, cervical dystonia is by no means rare. Exact prevalence rates are not available, but an estimated 60,000 – 160,000 Americans are living with cervical dystonia. In one study, only half of these patients reported being treated for their condition. Cervical dystonia often comes on in mid-life but can begin at any age, and typically affects women twice as frequently as men.
In addition to neck pain, many patients may manifest with a head tremor. Often patients (and physicians) assume that tremor is due to more common causes, such as Parkinson’s disease and essential tremor. However, isolated head tremor (meaning tremor involving the head and neck only and not involving the arms or legs) should be considered undiagnosed cervical dystonia until proven otherwise.
A tremor in cervical dystonia tends to be jerky and irregular and often is worse in the direction of the head away from the abnormal positioning. So, if cervical dystonia is causing a head turn to the right, tremor may be worst when the patient attempts to turn their head to the left.
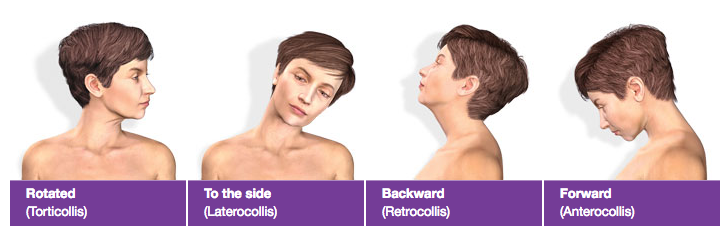
Cervical dystonia is known by many names, and the terminology can get confusing at times. The most common alternate name is spasmodic torticollis, but torticollis may also refer to the specific position of head turning to left or right, whereas head tilt (the ear coming down to the shoulder) is known as laterocollis. When the neck is extended (chin up) it is known as retrocollis, whereas neck flexion (chin down) is known as anterocollis.
There can be lateral (side to side) shift or sagittal (to the front or back) shift. There may also be shoulder elevation. Cervical dystonia is common in infants, and is often referred to as infantile torticollis. This typically resolves with physical therapy, rarely requiring surgery to release the muscles, and does not portend a risk of life-long cervical dystonia.
Diagnosis and Treatment of Cervical Dystonia
Typically, cervical dystonia is diagnosed based on the clinical exam, but in order to precisely define the type and severity of cervical dystonia, we perform a highly specialized rating scale, called the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS), typically with a video documentation after obtaining patient consent. In cases of dystonia involving other body parts in addition to the neck, further evaluation may be necessary to exclude other causes of dystonia. Genetic causes of dystonia are probably more common than we can currently assess for. Well-known specific genetic syndromes include DYT 1 generalized dystonia, dopa-responsive dystonia, and rapid onset dystonia-parkinsonism. In patients with young-onset dystonia, especially if there is involvement of the lower extremities and improvement after sleep, a levodopa trial is warranted: a dramatic response to levodopa would be expected if the diagnosis is dopa-responsive dystonia (aka Segawa syndrome). In some cases an MRI of the brain and blood or urine tests may be advised to exclude any other causes of adult-onset idiopathic (primary) cervical dystonia.

Ella received the mainstay of treatment for cervical dystonia, which is injection with botulinum toxin, such as Botox or Xeomin. Botulinum toxin — the same Botox that’s used for cosmetic purposes — is injected into the over-active neck muscles, causing a block of the communication between the nerve and the muscle. Thus, Botox calms down the specific muscles that cause the pulling and twisting, resulting in a more natural and neutral head position. Many patients are surprised to hear that Botox has a non-cosmetic use, but botulinum toxin injection has been used for neurological purposes for several decades, prior to its use for the relaxation of muscles that cause wrinkles.
We utilize EMG guidance during Botox injections to verify muscle activity and find the most active aspect of each muscle that is being injected. The number of units and injections may vary but typically ranges between 100 to 300 units, divided into 4 to 12 injections at a time. The entire procedure takes about 20-30 minutes in the clinic. Botox kicks in about 3-7 days after injection, and the duration of effect lasts about 10-14 weeks. Thus, effects of botulinum toxin injection are always temporary, and most patients return every 12 weeks for repeat injection. Conversely, if there are any side effects of the injection, they will resolve within a few weeks. Side effects of botulinum toxin injection typically occur due to spread of the toxin to other muscles, and may include neck weakness, trouble holding the head up, neck pain, swallowing difficulty and rarely slurred speech.
Untreated cervical dystonia can interfere with focus on work or school, resulting in reduced productivity, reduced working hours or even disability in many patients. In addition, a large majority of patients tell us that the dystonia impacts their social life and causes them to feel self-conscious about their appearance. By relaxing tense muscles, botulinum toxin injection results in a more natural head position, reduced neck pain, and reduced head tremor. In some patients, botulinum toxin injections are not sufficient to control the symptoms, and oral medications may be useful as additional treatment. Oral medications for dystonia may include benzodiazepines such as clonazepam, anticholinergics such as trihexiphenidyl, and muscle relaxants such as baclofen. All of these medications can be associated with muscle weakness, somnolence (sleepiness), dizziness, imbalance, and fogginess. In addition, trihexiphenidyl can cause dry mouth, nausea, constipation, urinary retention (inability to urinate) and confusion. Therefore, these oral medications are not considered first line over botulinum toxin injection.
A Surgical Option

Patients who do not respond to botulinum toxin injection or medication may be good candidates for deep brain stimulation surgery (DBS). DBS is like a pacemaker for the brain and results in non-permanent suppression of a deep part of the brain. Typically for dystonia, the brain structure called the globus pallidus interna (GPi) is targeted. This results in a release of brain activity, with reduction of the dystonia at the source of the problem (i.e., the brain, not the neck). DBS surgery results in long-term benefit of cervical dystonia, and the amount of stimulation given to the brain is modifiable, meaning that beneficial effect can be fine-tuned over several months. DBS surgery is brain surgery and requires the placement of tiny electrodes in the brain but it is a relatively safe procedure, with very low rates of complication (infection and bleeding being the main, very rare, risks). DBS surgery is performed in two stages: the implantation of the electrodes in the brain is done under awake conditions and the placement of the battery is done under general anesthesia as an outpatient procedure for a couple weeks subsequently.
Neurosurgeon, Dr. Jean-Philippe Langevin, neurosurgeon and director of the Restorative Neurosurgery and Deep Brain Stimulation Program at the Pacific Movement Disorders Center, is well experienced in implanting DBS systems. He is the only surgeon in Los Angeles currently offering the advanced STarFix Platform, a more comfortable, customized surgical experience called frameless DBS, in which the surgical hardware is personalized for each patient. During surgery, instead of having to wear a rigid frame that gets screwed into the operating table, immobilizing the head and neck, the frameless system is attached to the skull via previously placed fiducial markers, meaning that the head and neck can remain mobile. This translates into more comfort for the patient and a shorter surgery – by about 2-3 hours – while still maintaining precision.
At the post-operative visit, the battery (pulse generator) is turned on and DBS programming begins. While it may take a few weeks for maximal benefit, patients soon experience relaxation of dystonia and reduction of tremor and abnormal posturing. The DBS program is customized for each patient based on maximizing symptom reduction and minimizing side effects. Possible side effects of stimulation (which can be reduced by adjusting the DBS settings) include slurred speech, cognitive complaints, tingling, and imbalance. DBS for dystonia improves objective scores of dystonia movement and disability, but more importantly, it greatly improves quality of life including physical function, pain, general health and depression scores.
As experienced by Ella, many patients with cervical dystonia continue to suffer from their condition due to inappropriate or inadequate treatment, simply because of a lack of awareness of their condition by patients and even some physicians. If you suspect you or a loved one may have cervical dystonia based on abnormal positioning of the neck associated with tremor and/or pain, consider an evaluation by a movement disorders neurologist. Your quality of life could be greatly improved with appropriate diagnosis and state-of-the-art treatment.
For a consultation, please call 310-582-7433 to arrange a visit with Dr. Melita Petrossian. If you have already been treated for dystonia and you or your treating neurologist feels you may be a candidate for DBS surgery, please call us to arrange a multidisciplinary visit with Drs. Petrossian and Langevin at the same time.
For more information about cervical dystonia, please visit:
https://www.ninds.nih.gov/disorders/dystonias/detail_dystonias.htm
https://rarediseases.info.nih.gov/diseases/10668/cervical-dystonia
https://www.torticollis.org
www.pacificmovement.org
Read More About Dystonia
About the Author

Melita Petrossian
Melita Petrossian, MD, is Director of Pacific Movement Disorders Center and is a fellowship-trained neurologist with clinical interests and expertise in movement disorders such as Parkinson’s disease, essential tremor, dystonia, gait disorders, ataxia, myoclonus, blepharospasm, hemifacial spasm, Meige syndrome, spasticity, tics, and Tourette’s syndrome. She also specializes in Parkinson’s-related conditions such as Dementia with Lewy Bodies, progressive supranuclear palsy, multiple system atrophy, corticobasal degeneration, primary freezing of gait, and Parkinson’s disease dementia.
Last updated: August 8th, 2024


