A Month for Essential Tremor
by Melita Petrossian
March is National Essential Tremor Awareness Month!
Essential Tremor (ET) is a condition which truly deserves a full month to enhance awareness as it is about eight times more common than Parkinson’s disease. A neurological movement disorder that presents with symptoms of tremor, ET is the most common movement disorder affecting more than an estimated 7 million Americans and as much as 4% of the U.S. population over the age of 65. Unfortunately ET is not nearly as well known as PD nor is ET research anywhere as well funded. Many patients who come to us worried about having PD because of their tremor are relieved to hear that their symptoms are due to ET. Yet ET can cause significant impacts on quality of life and social functioning that can be just as disruptive. A comparison of essential tremor and Parkinson’s disease shows various differences in signs and symptoms.
Originally known as “benign essential tremor”, the term “benign” was dropped because specialists realized that there could be cases where severe tremor affected activities of daily living. The term “essential” in this case refers to the fact that the “essence” of the condition is tremor.

ET typically causes a tremor affecting both upper extremities when holding a posture or with action, meaning when moving the arm. ET can also cause shaking in the head or voice. Patients may first notice the tremor when holding the newspaper, smart phone, or trying to carry a cup on a saucer. The tremor can affect – depending on the severity – ability to write, type, pour liquids, use a spoon, shave, put on earrings, and button buttons. For people whose line of work requires a high degree of fine motor control, such as jewelers, dentists, and surgeons, even a mild tremor may be disabling.
Tremor can also have social impacts even when there is no real effect on activities of daily living. For example, patients such as consultants and actors may have a high degree of scrutiny on their appearance, and colleagues may erroneously attribute tremor to anxiety. This can of course also affect people in other professions as well. Part of the issue here has to do with the lack of awareness about the condition and patients may not wish to share details of their neurological disease for fear of bias.
The vast majority of patients with ET have a very slow progression of their condition. Onset of ET has a bimodal distribution. This means about half of patients have onset in their youth (20’s or even younger), and the other half have onset in their 40’s, 50’s, or 60’s. Those who have onset in their youth are more likely to have family history than those with onset later in life. Because of the very slow progression, many patients may have mild tremor for decades before it becomes a major problem, and some never progress to severe levels.
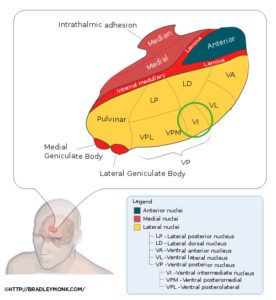
ET is related to the brain’s tremor generator, which is in the ventral intermediate (VIM) nucleus of the thalamus (a small collection of cells in a deep part of the brain). Naturally the other parts of the brain inhibit (limit the activity of) the tremor generator, but in ET there is thought to be a degeneration of these parts. However, unlike in Alzheimer’s or Parkinson’s disease, the exact areas of degeneration have not been identified, nor have there been specific proteins implicated in the process.
Diagnosis of ET is primarily based on the clinical exam. Blood tests may be done to exclude other causes such as an overactive thyroid. The patient’s medication list is reviewed to make sure tremor is not being caused by medications. In cases where the exam does not provide a definitive diagnosis, the DaTscan is FDA approved and effective in differentiating between tremor caused by ET and that caused by PD. This is a non-invasive test available here at Providence Saint John’s Health Center.
Unfortunately, there are no cures or treatments that prevent progression of the condition. This means that treatment is focused only on symptomatic improvement. Therefore, many patients with mild ET opt against medication and rely on coping techniques, such as using two hands to pour liquids, using a mug instead of a cup, using magnetic buttons, or block printing instead of cursive writing. Patients who desire medication options on an as-needed basis may use a beta-blocker such as propranolol, which blocks the “fight-or-flight” sympathetic nervous system response and reduces tremor temporarily. This can be an effective option for those whose tremor is only bothersome in certain social situations. Others who have more difficulty can take propranolol daily, or can try other medications such as primidone, which is an anti-seizure medication. There have not been advances recently to medication options; many have been tried, but none have been shown to be more effective than primidone and propranolol. These medications do not stop the tremor but may reduce the amplitude slightly, improving quality of life. However, they can cause (temporary) side effects such as dizziness and their efficacy may wane over the years.
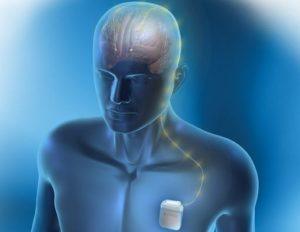
More advanced treatment options include deep brain stimulation (DBS) surgery, targeting the VIM, which can improve tremor by around 75%, and is reversible and adjustable over the years. People with severe tremor who are generally medically healthy with normal MRI but have had poor response to medication, may be excellent candidates for DBS. The stimulation works by (paradoxically) inhibiting the tremor-generating part of the brain. Electrodes are placed deep inside the brain and wires are connected – all under the skin – to a battery that is located under the skin of the chest, similar to a pacemaker. While this may sound like science fiction, DBS is a very effective and well established procedure approved by the FDA and in usage since 1997.
Pacific Movement Disorders Center at Pacific Neuroscience Institute located at Providence Saint John’s offers a newer technique during the procedure itself, called the frameless approach. This results in shorter procedure time and less discomfort during the procedure, while maintaining an excellent degree of accuracy.
There are other treatment options for advanced ET such as gamma knife radiosurgery. This is a one-time procedure that is not modifiable and whose effectiveness and possible side effects are unknown for several months. Another promising treatment option is focused ultrasound, which is a non-modifiable, one-time procedure, the effects of which are immediate. This is performed by entraining hundreds of beams of ultrasound on the VIM, heating up the VIM and creating a tiny lesion. This is done under MRI guidance with the patient awake so that the exam is monitored for reduction in tremor and absence of side effects. Focused ultrasound was FDA approved in July 2016 and while not yet in Southern California, it is available at Providence’s location at Swedish Hospital in Seattle.
For more information and support visit the International Essential Tremor Foundation. For consultations and second opinions on diagnosis and management of tremor of all causes please contact us at Pacific Movement Disorders Center at 310-582-7433.
About the Author

Melita Petrossian
Melita Petrossian, MD, is Director of Pacific Movement Disorders Center and is a fellowship-trained neurologist with clinical interests and expertise in movement disorders such as Parkinson’s disease, essential tremor, dystonia, gait disorders, ataxia, myoclonus, blepharospasm, hemifacial spasm, Meige syndrome, spasticity, tics, and Tourette’s syndrome. She also specializes in Parkinson’s-related conditions such as Dementia with Lewy Bodies, progressive supranuclear palsy, multiple system atrophy, corticobasal degeneration, primary freezing of gait, and Parkinson’s disease dementia.
Last updated: March 6th, 2024