

Supporting a Cure for Brain Cancer
by Zara Jethani
A review of new research and treatments for brain cancer in 2016
TJ was diagnosed with a stage III Astrocytoma brain tumor at the age of 14. Even after four brain surgeries, several courses of radiation over 5 years, many kinds of chemotherapy, experimental treatments, alternative treatments, bone marrow transplant, and gamma knife he passed away 4 days before his 19th birthday in 2007.
With no predictable risk factors linked to the development of brain tumors, we as a medical and research community must forego prevention for the present and focus our efforts on developing cures.
In his book, Emperor of All Maladies, author Dr. Siddhartha Mukherjee asks, “Is cancer’s end conceivable in the future? Is it possible to eradicate this disease from our bodies and societies forever?”
At Pacific Brain Tumor Center we approach this from a very human and personal point of view. What can we do for each patient who comes in to see us? How can we prolong life – help cure – this patient? We continue to provide the highest levels of neurosurgical and neuro-oncological treatments to our patients. Each kind of brain cancer is distinct and as a disease collective, cancer cannot be viewed as a single entity therefore neither can the cure.
Santosh Kesari, MD, PhD, chair of the Department of Translational Neurosciences and Neurotherapeutics at Saint John’s Cancer Institute and Pacific Neuroscience Institute at Providence Saint John’s Health Center constantly evolves, incorporating practice-changing treatments into the options he offers to patients with brain cancer.
Thinking out of the box has generated therapies such as Voyager (from Nativis) and Optune (from Novacure) that use tumor treating low-intensity alternating electrical fields to disrupt cancer cell growth, which now have wider applications for patients newly diagnosed with glioblastoma multiforme (GBM) – a deadly disease with a prognosis of only about 14 months.
At SNO2016, Dr. Kesari discussed including Optune in the standard of care. “Recent long-term analysis data on the Novocure Optune study called EF-14 shows that there is sustained improvement in survival at four years,” says Dr. Kesari who was one of the investigators for the clinical trial. Optune used along with temozolomide chemotherapy demonstrated a significant increase in progression-free and overall survival compared to patients treated with temozolomide alone. In addition, EF-14 patients treated with Optune together with temozolomide experienced a 70 percent improvement in survival rate at four years compared to patients treated with temozolomide alone.
Precision treatment advances in minimally invasive surgical techniques lead to more favorable outcomes. The use of stereotactic radiosurgery (SRS) offers focused treatment of difficult to treat brain cancers that cannot be reached effectively by chemotherapy due to the blood brain barrier (BBB).

The arc of treatment improvement is clear. At the Precision Cancer Care in 2016 meeting sponsored by Saint John’s Cancer Institute, Dr. Daniel Kelly, PNI director said, “It used to be that once brain mets were detected, the only thing you could provide the patient was hope and prayer. Then with minimally invasive endoscopic surgery (often through the nose or optic orbit) and whole brain radiation therapy you could give them a survival of 6 months. Now there are targeted radiotherapy systems available that go even further.”
Neuro-oncology research focusing on individualized treatments is one of the ways forward in stopping the spread of cancer. “For over 40 years, the American Brain Tumor Association has provided critical funding of research in the pursuit of breakthroughs in brain tumor diagnosis, treatment and care,”says Phung Tran, Manager of Marketing & Communications at the American Brain Tumor Association (ABTA). “We have funded nearly $30 million in brain tumor research, which has led to a better understanding of the genetic makeup, signaling and microenvironment of brain tumors; new drug development and novel treatments; and helped to enhance the quality of life for brain tumor patients,” she adds.
The results of these kinds of research and clinical trials can greatly enhance disease-free and progression-free survival resulting in improved quality of life. DNA sequencing technologies can shed light on why certain patients become exceptional responders to otherwise ineffective therapies.
Treatments that look at patient genetics and medical histories promise to be more effective and cause fewer side effects than more traditional therapies developed for a generalized population of patients. The idea of “basket trials” is that a single treatment regimen can be used across different cancer types because of similar cell characteristics or mechanisms. Dr. Kesari works with patients to ascertain if off-label usage is appropriate for them.
Exploring the idea of delivering chemotherapy in a effective way, Dr. Kesari participated in a recent study using the chemotherapeutic drug, paclitaxel which when linked to a specific peptide, was able to cross the BBB allowing it to reach its intracranial tumor target. “The days of non-specific chemotherapy is in the past,” said Dr. Steven J. O’Day, Professor of Medical Oncology and Director of Immuno-Oncology at Saint John’s Cancer Institute. “The immune-oncology revolution is prevalent across all cancers today.”
Immunotherapy options include checkpoint inhibitors, which help the immune system work more effectively. Immuno-vaccines can deliver targeted gene therapies to reverse the effects of specific mutations in tumor cells and viral therapy offers a precise method to destroy cancer cells using methodologies such as oncolytic virus-drug combinations.
Approximately 10-30% of brain tumors are due to brain metastases from other primary tumors and account for 150,000-200,000 people in the United States being diagnosed with brain metastases each year. But how do we know which tumor cells will become metastatic? Researchers think that certain cell characteristics could potentially predict metastatic properties such as proliferation and “stickiness”.

Natsuko Nomura
Studies that look for predictive factors like the presence of RSK2 kinase may lead to the development of inhibitors which could reduce recurrence and metastatic activity. The study published in Oncotarget showed that a protein called RSK2 increases in many patients with glioblastoma. The protein pushes glioblastoma cells into surrounding healthy brain tissue making it difficult to remove the tumor by surgery, which contributes to high recurrence and poor survival rates in patients. The invading glioblastoma cells are less sensitive to current standard therapies but inhibiting RSK2 stops invasion of the tumor cells and enhances the effectiveness of standard chemotherapy in tumor cells obtained from patients. “This study paves the way for development of new brain cancer therapies focused on RSK2 inhibitors for brain invasion,” said co-author Dr. Kesari.
For TJ’s parents, Diane and Larry Peacock, these advances were not available to their family, but Diane made a pledge, “I promised my son and myself that I would spend the rest of my life making him proud and carrying on his battle so that some day we can prevent another family from suffering the way we, and many others have suffered.” To this end, TJ’s Dream Team was founded with the aim of raising funds, 100 percent of which go toward brain cancer research. In November, Pacific Neuroscience Institute and Dr. Kesari were the recipients of the proceeds this year.
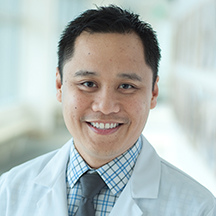
At Pacific Neuroscience Research Center, Dr. Marlon Saria’s quality and outcomes research is leading to a new way of supporting family caregivers. “In the age of precision medicine, the care of the caregiver is several years behind the powerful advances in the diagnosis and treatment of brain cancer. Our team believes that a well-being assessment of family caregivers needs to be integrated into the standard of care”.
Aware of the real toll that cancer takes on patients and their caregivers, ABTA’s Phung Tran states, “Since its inception, the ABTA has been providing comprehensive resources that support the complex needs of brain tumor patients and caregivers.” The ABTA continues to provide and pursue answers for brain tumor patients and their caregivers because of donations. This holiday season one of the ways to support a cure for brain cancer is by sending an e-card.
About the Author

Zara Jethani
Zara is the marketing director at Pacific Neuroscience Institute. Her background is in molecular genetics research and healthcare marketing. In addition, she is a graphic designer with more than 20 years experience in the healthcare, education and entertainment industries.
Last updated: May 6th, 2021
