Delving Into Cavernous Malformations
by Zara Jethani
What are Cavernous Malformations?
Cavernous malformations (CMs), also known as cavernomas or cavernous angiomas, are clusters of abnormal, dilated blood vessels that can form in the brain, spinal cord, or other parts of the body characterized by distended blood-filled “caverns.” Unlike normal blood vessels, these clusters do not involve significant tissue between the blood vessels, creating a “cavernous” appearance. Although often benign, cavernous malformations can cause various neurological symptoms and complications. Here we delve into the causes, symptoms, diagnosis, and treatment options for this condition.
Cavernous malformations form in clusters that resemble small mulberries and often are characterized by:
- Slow blood flow: This can lead to small, repeated hemorrhages, potentially causing progressive symptoms.
- Location matters: When a cavernous malformation is in a critical area of the brain, even small bleeds can result in significant neurological effects.
- Varied symptoms: Some patients may experience no symptoms, while others may have severe, life-altering issues.
Causes of Cerebral Cavernous Malformations
The exact cause of cavernous malformations remains unclear, but they can be categorized into two main types: sporadic and familial.
- Sporadic Cavernous Malformations: These occur randomly and usually present as a single lesion. They are thought to be caused by mutations in the genes involved in blood vessel formation and stability.
- Familial Cavernous Malformations: These are inherited and typically involve multiple lesions. About 20-30% of cases are inherited and caused by mutations in one of three known genes: KRIT1, CCM2, or PDCD10. If you have a familial form, there’s a 50% chance of passing the condition to your children. People with the genetic form often develop multiple cavernous malformations.
Brain Symptoms of CMs
Symptoms of cavernous malformations can vary widely depending on their location, size, and whether they bleed (hemorrhage). Some individuals remain asymptomatic, while others may experience severe neurological deficits. Common symptoms include:
- Headaches: Recurrent and sometimes severe headaches are a frequent symptom, particularly if the malformation is in the brain.
- Seizures: These are common, especially if the cavernoma is located in the cerebral cortex.
- Neurological Deficits: Depending on the lesion’s location, symptoms can include weakness, numbness, difficulty with coordination and balance, vision problems, and speech difficulties.
- Hemorrhage: Bleeding can cause sudden and severe symptoms, including acute headache, nausea, vomiting, and neurological deterioration.
Diagnosis of Cavernomas
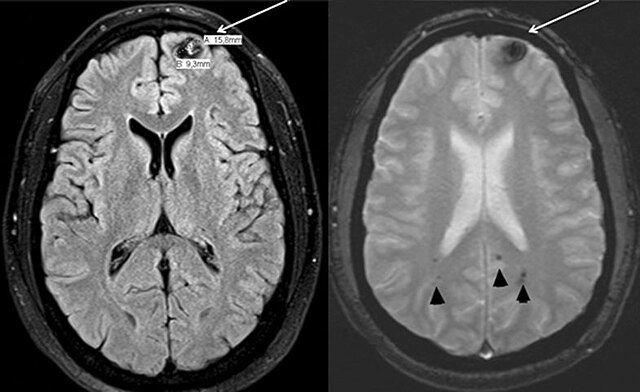
Diagnosing cavernous malformations typically involves imaging studies. The most effective methods include:
- Magnetic Resonance Imaging (MRI): This is the gold standard for diagnosing CMs. MRI can reveal detailed images of the brain or spinal cord, showing the size, location, and number of lesions.
- Computed Tomography (CT) Scan: While less sensitive than MRI, CT scans can detect larger lesions and hemorrhages.
- Genetic Testing: For individuals with a family history of CMs or multiple lesions, genetic testing can identify mutations associated with the condition.
Treatment of CMs
The treatment approach for cavernous malformations depends on the patient’s symptoms, the lesion’s size and location, and the risk of hemorrhage. Options include:
- Observation: In asymptomatic or minimally symptomatic cases, regular monitoring with periodic MRI scans may be recommended.
- Medication: Anti-seizure medications can help manage seizures associated with CMs.
- Surgical Removal: For symptomatic lesions causing significant neurological deficits or recurrent hemorrhages, surgical resection may be necessary. Advances in microsurgical techniques and imaging have improved the safety and efficacy of these procedures.
- Stereotactic Radiosurgery: This non-invasive procedure uses focused radiation to shrink the malformation over time. It is typically reserved for deep-seated lesions that are difficult to access surgically.
In Summary
Cavernous malformations are complex vascular lesions that can present a wide range of symptoms and complications. Early diagnosis and appropriate management are crucial to mitigate risks and improve quality of life for affected individuals. Advances in imaging and surgical techniques continue to enhance the understanding and treatment of this condition. If you or a loved one is experiencing symptoms suggestive of a cavernous malformation, consulting a healthcare professional for a thorough evaluation is essential.
Cavernous Malformation Specialists at Pacific Neuroscience Institute®
Contact Us
At Pacific Neuroscience Institute, a team of experts sees cavernous malformation patients at four locations across Southern California. The Pacific Stroke and Neurovascular Center’s state-of-the-art facilities are located at:
Providence Saint John’s Health Center
2125 Arizona Ave., Santa Monica, CA 90404
310-829-8319
Providence Little Company of Mary Medical Center Torrance
4201 Torrance Blvd., Suite 520, Torrance, CA 90503
424-212-5340
Providence Saint Joseph Medical Center
501 S. Buena Vista Ave., Burbank, CA 90505
818-847-6049
Providence Holy Cross Medical Center
15031 Rinaldi St, Mission Hills, CA 91345
818-847-6570
Is a Cavernoma Considered a Disability?
A cavernous malformation is a cluster of abnormal blood vessels that can occur in the brain or spinal cord. Whether a cavernous malformation is considered a disability depends on its impact on daily life. Some patients with cavernous malformations experience no symptoms and require no treatment, while others may have seizures, neurological deficits, or headaches.
Key factors that determine if a cavernous malformation qualifies as a disability include:
- Severity and frequency of symptoms
- Impact on physical and cognitive abilities
- Treatment requirements and potential complications
When these malformations cause significant limitations in daily activities or require ongoing medical care, they may be classified as a disability. However, each case is unique, so it’s essential to consult with a healthcare provider to understand your specific situation.
What is the difference between aneurysm and cavernoma?
A cavernous malformation and an aneurysm are both vascular abnormalities, but they differ significantly in structure and risk. A cavernous malformation consists of abnormal, dilated blood vessels forming a cluster, often compared to a small berry. These malformations are usually low-pressure and slow-growing, often causing seizures, headaches, or neurological symptoms.
In contrast, an aneurysm is a bulge or ballooning in the wall of a blood vessel, typically an artery, due to weakness. Aneurysms carry a higher risk of rupture, leading to severe bleeding, stroke, or even death.
Key differences include:
- Structure: Cavernous malformations are clusters of blood vessels; aneurysms are bulges in arteries.
- Risk: Cavernous malformations have a lower risk of sudden rupture compared to aneurysms.
- Symptoms: Both can cause neurological issues, but aneurysms often present more acutely if they rupture.
What are the long term effects of cavernomas?
Cavernous malformations can have several long-term effects, depending on their location, size, and whether they cause symptoms. These malformations may lead to recurrent headaches, seizures, or neurological deficits such as weakness, vision problems, or difficulty with coordination. Some cavernous malformations bleed intermittently, which can result in progressive neurological deterioration over time.
Key long-term effects include:
- Seizures: Often requiring ongoing medication management.
- Neurological deficits: Such as weakness, sensory changes, or speech difficulties.
- Cognitive impairment: In cases where cavernous malformations affect critical areas of the brain.
In some cases, these malformations remain stable and asymptomatic, but others may worsen, leading to a gradual decline in function.
What is the success rate of cavernoma surgery?
Cavernoma surgery, performed to remove cavernous malformations, generally has a high success rate, particularly when symptoms are severe or bleeding occurs. Success depends on the malformation’s location, size, and the patient’s overall health. Surgeons achieve favorable outcomes in most cases, especially when the cavernous malformation is accessible and located in a non-eloquent area of the brain.
Key success factors include:
- Symptom Relief: Surgery often reduces or eliminates symptoms such as seizures or neurological deficits.
- Bleeding Prevention: Removing the malformation reduces the risk of future hemorrhages.
- Low Recurrence: Recurrence of the cavernous malformation is rare after successful removal.
However, surgery carries risks, including potential damage to surrounding brain tissue, especially in delicate areas. Patients should discuss these risks with their neurosurgeon to understand the benefits and potential complications specific to their case. Long-term outcomes are generally positive, with many patients experiencing significant improvement.
Can a cavernoma cause a stroke?
Cavernous malformations can lead to stroke-like symptoms, but they differ from typical strokes caused by blockages or large vessel hemorrhages. These malformations are clusters of abnormal blood vessels that may bleed slowly, resulting in small, repeated hemorrhages. When a cavernous malformation bleeds, it can cause localized brain damage, leading to symptoms similar to those of a stroke, such as weakness, numbness, or difficulty speaking.
What triggers cavernomas?
Cavernomas, also known as cavernous angiomas or cavernous malformations, are clusters of abnormal blood vessels typically found in the brain or spinal cord. The exact cause of cavernomas isn’t always clear, but several factors can trigger their formation or lead to their symptoms becoming apparent:
- Genetic Factors: Some people inherit a predisposition to develop cavernomas. Familial cavernous malformation, caused by mutations in specific genes (like CCM1, CCM2, or CCM3), can lead to multiple cavernomas. This genetic form is passed down in an autosomal dominant pattern, meaning a person only needs one copy of the mutated gene from one parent to be at risk.
- Developmental Factors: Cavernomas can develop sporadically without any family history. These sporadic cavernomas are usually solitary and may form as a result of abnormal blood vessel development during embryonic growth.
- Radiation Therapy: In some cases, cavernomas can form as a side effect of radiation therapy, particularly in the brain. This is more common in people who have undergone radiation therapy during childhood.
- Trauma: Although rare, head trauma has been suggested as a potential trigger for the formation of cavernomas or the hemorrhage of an existing one.
- Hormonal Changes: Some studies suggest that hormonal changes, such as those occurring during pregnancy, can exacerbate symptoms or lead to the detection of a previously asymptomatic cavernoma.
- Aging: As people age, the risk of symptoms or hemorrhage from a cavernoma can increase, possibly due to the cumulative effects of small, undetected bleeding events over time.
Cavernomas may remain asymptomatic for years and are often discovered incidentally during brain imaging for other conditions. However, when they do cause symptoms, it’s usually due to bleeding (hemorrhage), seizures, headaches, or neurological deficits depending on their location.
About the Author

Zara Jethani
Zara is the marketing director at Pacific Neuroscience Institute. Her background is in molecular genetics research and healthcare marketing. In addition, she is a graphic designer with more than 20 years experience in the healthcare, education and entertainment industries.
Last updated: October 9th, 2024