Endoscopic Pituitary Adenoma Surgery: Safety First
by Daniel F. Kelly
Primum non nocere … “First do no harm”
Whether this phrase comes from the Hippocratic Oath or subsequent medical scholars is debatable but it remains one of the guiding principles in medicine.
Pituitary Adenomas
At Pacific Neuroscience Institute and our Pacific Pituitary Disorders Center, this concept of “safety first” is paramount when it comes to removing pituitary adenomas, and related tumors such as craniopharyngiomas, Rathke’s cleft cysts, chordomas and some midline meningiomas (not cancerous) growths of the gland itself.
The great majority of symptomatic pituitary adenomas (the vast majority of which are benign and non-cancerous), require surgical removal as first-line treatment.
Common symptoms include:
- Loss of hormonal function (hypopituitarism)
- Excess hormone production
- Vision loss
- Headaches
The only subset of adenomas that can be reliably treated without surgery are prolactinomas, typically with a medication called cabergoline (a dopamine agonist).
The Key Goals of Pituitary Adenoma Surgery Are:
- Complete tumor removal
- Preservation or restoration of gland function
- Restoration of vision (if vision loss is a symptom)
- Avoidance of surgical complications
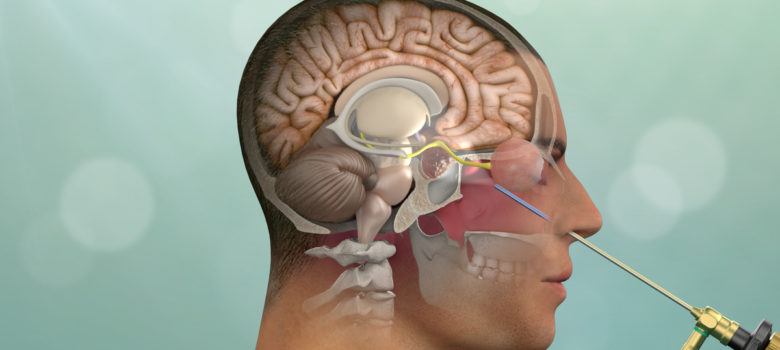
Reaching Tumors of the Pituitary Gland
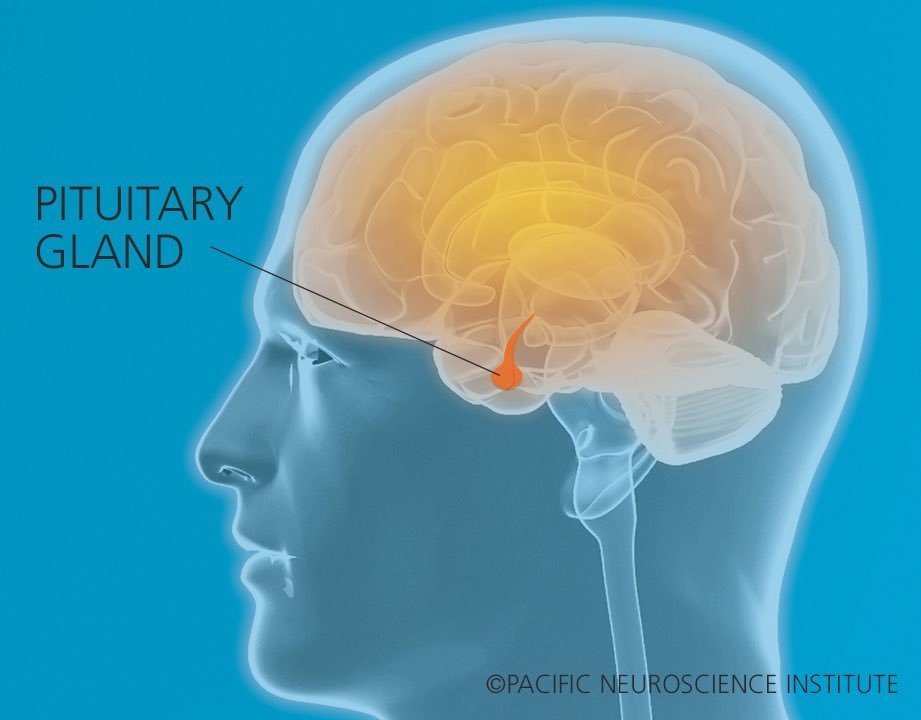
Given where the pituitary gland is located, meeting this challenge is no small issue – the small pituitary gland, is located below the brain in the skull base, in an area called the sella turcica.
It is surrounded on either side by the paired carotid arteries, and above by the optic nerves, optic chiasm and brain itself, and is attached to the brain itself by a thin delicate neuro-vascular connection called the pituitary stalk or infundibulum.
With all these critical structures within such a tiny space, extensive anatomical understanding, surgical experience, and careful planning of surgery are required to achieve optimal outcomes and to “do no harm” to our patients.
Safety First
At PNI with over 1000 endoscopic endonasal surgeries performed for pituitary adenomas and related conditions over the last 13 years, and over 80 peer-reviewed publications related to the pituitary gland and endoscopic surgery, our focus on “Safety First” has paid off for our patents. In looking back at our outcomes, the rates of major complications have been extremely low.
In a soon-to-be-published manuscript, of over 500 cases of endoscopic pituitary surgery operations, our risks of major complications was <1% for vision worsening, stroke or other neurological decline, carotid or other blood vessel injury, blood clot, meningitis, deep vein thrombosis, pulmonary embolism, loss of sense of smell and death.
A postoperative cerebrospinal fluid leak occurred in only 1.4% of cases.
In patients with preoperative vision loss, improvement was documented in almost 90% and in patients with preoperative headaches, improvement or resolution occurred in over 90%.
Tumor removal rates were also high, achieving total or near total removal in 90% of patients with endocrine-inactive adenomas. Notably of all these cases, over 20% had prior surgery performed at another institution.
A Team Approach to Minimally Invasive Surgery
Performing safe and effective surgery for patients with pituitary tumors, tumors of the skull base and pituitary tumors requires a dedicated and experienced team of specialists. Over the last two decades, minimally invasive approaches to reach these often difficult-to-access tumors has flourished largely due to advances in neuro-anatomical understanding as well as refinements in instrumentation including the high-definition endoscope, ultrasound and surgical navigation.
How We Perform Surgery
In over 98% of cases, pituitary adenomas are removed via the nose (endonasal endoscopic route). At PNI our surgical philosophy is to maximize tumor removal while minimizing risk of collateral damage and complications through experience and use of the best available technology including high-definition, endoscopy, intraoperative navigation and the Doppler probe for blood vessel localization.
Surgery Recovery
Most patients undergoing endonasal or keyhole craniotomy removal of a tumor impacting vision or eye movements are in the hospital for only one or two nights and are back to full activities within 3 weeks after surgery.
Unique Team Of Specialists Under One Roof
Our comprehensive team approach allows patients with pituitary tumors to be evaluated by multiple specialists under one roof in our new PNI Clinic in Santa Monica. For example, in one visit, our patients can see Dr. Howard Krauss (neuro-ophthalmology), Drs. Daniel Kelly or Garni Barkhoudarian (neurosurgery), Dr. Chester Griffiths (ENT), and Dr. Katherine Araque (endocrinology).
Additional appointments may also be arranged for the same visit or on another day with our neuro-oncologists and our radiation oncologists.
PNI Pituitary Experts
Neuro-ophthalmology
Radiation Oncology
Interventional Neuroradiology
Additional Resources
As detailed in our publications, our PNI team has performed surgery on hundreds of patients with vision and/or eye movement deficits. These papers highlight the use of various keyhole approaches for such tumors including the endonasal and supraorbital route. Examples of these approaches are also in our keyhole surgery video library.
Contact Us
To learn more about our Pituitary Disorders Center and endoscopic endonasal surgery, or to get a second opinion about a pituitary tumor, schedule a consultation online or call 310-582-7450.
About the Author

Daniel F. Kelly
Daniel F. Kelly, MD, is the Director of the Pacific Brain Tumor and Pituitary Disorders Centers at Providence Saint John’s Health Center in Santa Monica, CA. Considered to be one of the top neurosurgeons in the U.S., Dr. Kelly is internationally recognized in the field of minimally invasive keyhole surgery for brain, pituitary and skull base tumors. He continues to focus his efforts on advancing innovative treatments for patients, providing fellowship training in minimally invasive neurosurgery, and patient education and support.
Last updated: June 6th, 2022