Meningioma
What is a Meningioma?
A meningioma is a type of tumor that arises from the meninges, which are the protective membranes that surround the brain and spinal cord. It is typically a slow-growing, usually benign tumor, derived from the cells of the arachnoid cap cells or the meningeal cells themselves. Meningiomas account for the majority of primary brain tumors, representing about 30% of all intracranial tumors. Meningiomas are the most common primary brain tumor. Fortunately, most are benign and slow-growing although up to 10% can grow rapidly. They are more common in women than men and can occur in all ages but are typically seen in middle-aged and older adults. Most meningiomas needing surgery can be removed through one of several minimally invasive keyhole approaches.
The exact cause of meningiomas is not fully understood, but certain risk factors have been identified, including prior exposure to radiation and certain genetic syndromes, such as neurofibromatosis type 2. However, in the majority of cases, the underlying cause remains unknown.
Meningiomas can occur at any age but are more commonly diagnosed in adults, particularly females. They can develop in various locations within the skull and spinal cord, including the convexity of the brain, the falx cerebri, the skull base, and the spinal meninges. Depending on their location and size, meningiomas may exert pressure on adjacent structures, leading to a range of neurological symptoms.
Symptoms of Meningioma
Symptoms of a meningioma are entirely dependent upon their location. Those arising in the skull base near the pituitary gland, optic nerves and cavernous sinus often cause visual loss or double vision. Those that arise along the top or side of the head pushing in on the brain surface may cause weakness, vision loss, personality changes, seizures and headaches. Those in the posterior fossa can cause facial pain or weakness, double vision, difficulty swallowing, imbalance and incoordination.
Meningioma Treatment
The treatment approach for meningiomas depends on several factors, including tumor size, location, and the patient’s overall health. In many cases, observation with regular monitoring may be sufficient for small, asymptomatic meningiomas that are not rapidly growing. However, if treatment is necessary, surgical resection is the primary treatment modality. The goal of surgery is to remove the tumor completely while minimizing damage to healthy brain tissue.
The optimal treatment for most symptomatic meningiomas is maximal safe surgical removal. Fortunately, most meningiomas can be removed through one of several minimally invasive keyhole approaches. At PNI, we have one of the world’s largest experiences with minimally invasive meningioma removal and provide comprehensive long-term care for our meningioma patients. In some instances, especially with invasive meningiomas in the skull base, complete removal may not be possible and additional therapy may be needed in the years following surgery, such as focused radiation.
Growth Patterns
Meningiomas may arise from any meningeal surface and are typically attached to the dura (outer layer of the meninges). Common meningioma locations are the convexity (top of the head), temporal region (sphenoid wing), cavernous sinus, frontal fossa (olfactory groove, tuberculum sella), internal dural surfaces including the falx and tentorium, and in the posterior fossa adjacent to the brainstem and cerebellum, as well as around the foramen magnum (where the brainstem transitions to the spinal cord).
Meningioma Neurosurgeons and Specialists
At the Pacific Neuroscience Institute in Santa Monica, CA we have one of the world’s largest experiences treating all such parasellar meningiomas with keyhole and endoscopic approaches as well as treating residual, recurrent and atypical meningiomas. By incorporating cutting edge technology and instrumentation with proven surgical experience, we make meningioma surgery safer, less invasive and more effective.
Overview
Meningiomas are the most common benign brain tumor although up to 10% can exhibit more aggressive growth patterns.
Meningioma Grading
Meningiomas are classified by the World Health Organization into 3 grades based on their growth pattern and histology:
- Grade I (typical – 90%)
- Grade II (atypical – 6-9%)
- Grade III (anaplastic 1-3%)
These tumors arise from arachnoidal cap cells in the brain coverings (meninges). They are more common in women than men and can occur in all ages but are typically seen in middle-aged and older adults.
They may arise from any meningeal surface and are typically attached to the dura (outer layer of the meninges) but can also occur in the cerebral ventricles.
Meningiomas of the midline skull base that arise near the pituitary gland include planum sphenoidale, tuberculum sella, clinoidal, optic canal, cavernous sinus, Meckel’s cave and petroclival meningiomas.
Some highly invasive and extensive meningiomas may extend into multiple compartments and into the sella itself, surrounding the pituitary gland.
Meningioma Symptoms
Midline meningiomas of the skull base that arise above the pituitary gland (tuberculum sellae), or in front of the pituitary gland (planum sphenoidale), typically cause progressive visual loss from optic nerve and optic chiasm compression.
They may also cause:
- Headache
- Double vision
- Loss of pituitary function
Meningiomas that extend into the cavernous sinus may cause double vision (diplopia) and those that extend into the region called Meckel’s cave (below the cavernous sinus), may cause facial numbness or tingling.
Some large petroclival meningiomas that arise in front of the brain stem, may cause:
- Double vision
- Loss of vision
- Facial numbness
- Difficulty walking
- Difficulty swallowing
- Urinary incontinence
- Headache
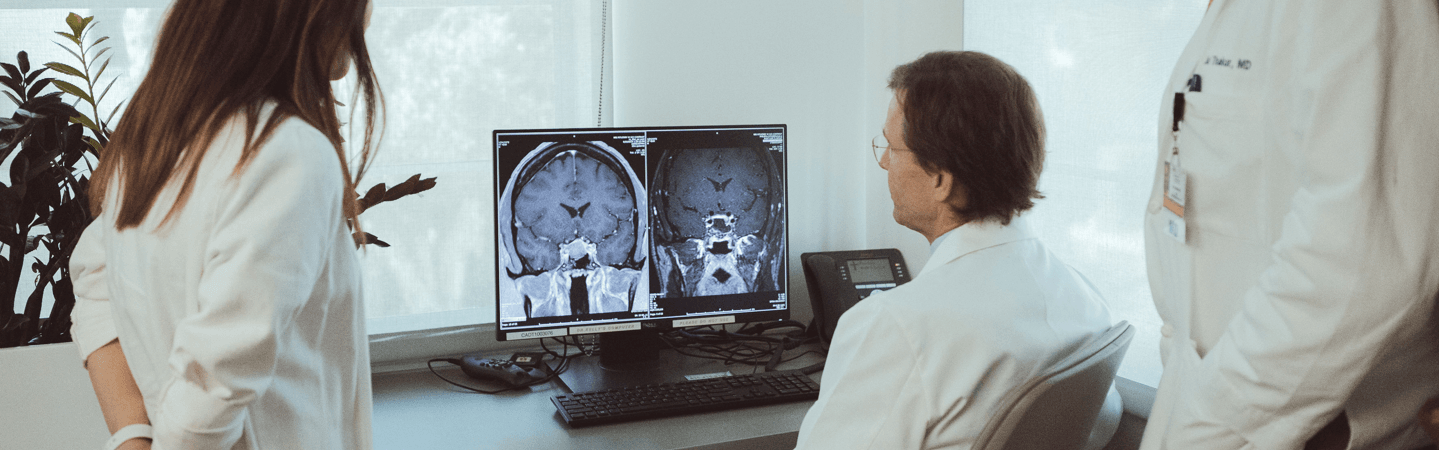
Diagnosis
Meningiomas are best diagnosed by an MRI of the brain with gadolinium, or by a CT scan of the brain with contrast.
Midline skull base meningiomas
For midline skull base meningiomas adjacent to the pituitary gland, a focused MRI of the pituitary region, or orbits is often indicated to obtain better anatomical detail of a meningioma.
Other tests may also be needed such as angiography (a CT angiogram or an MR angiogram), visual field tests, and pituitary hormonal tests.
Meningioma Treatment
Meningioma Surgery
Symptomatic tuberculum sellae or planum sphenoidale meningiomas are typically treated by surgical removal through either a supraorbital eyebrow or an endoscopic endonasal approach.
Our Center Director, Dr. Daniel Kelly has been one of the pioneers in removing tuberculum sellae meningiomas through an endoscopic endonasal approach and comparing this approach to the supraorbital approach.
Advantage of endoscopic endonasal surgery
The advantage of the endonasal approach over a transcranial approach is that brain retraction is not necessary and manipulation of the optic nerves and chiasm is minimized.
However, for larger tumors (over 3 cms) or those that extend far off the midline, the supraorbital eyebrow approach is an excellent minimally invasive alternative.
With either approach, vision typically improves and pituitary hormonal function is usually preserved. For some larger meningiomas in this region, a more conventional pterional (fronto-temporal) craniotomy may be needed.
For invasive parasellar meningiomas that involve the cavernous sinus, Meckel’s cave, sella and/or petroclival region, endoscopic endonasal tumor debulking and bony decompression is a reasonable treatment option that we often use and often follow with focused stereotactic radiotherapy.
Radiosurgery (SRS) or Stereotactic Radiotherapy (SRT)
Meningiomas of the cavernous sinus, Meckel’s cave, sella tursica and petroclival region cannot be completely removed in over 50% of cases. For meningiomas of the tuberculum sellae or planum sphenoidalea, complete tumor removal rates are significantly higher.
With incomplete removal or if a tumor re-grows stereotactic radiotherapy (SRT) or Stereotactic Radiosurgery (SRS), are often needed to halt further tumor growth.
The tumor control rate with SRS or SRT is quite high with over 90% of patients having no further tumor growth. Complications of SRS or SRT such as visual loss or brain injury are rare.
Doctors and Specialists Who Treat Meningiomas
Patient Stories
Hear from our patients. Read their stories of courage and caring.
Olfactory Groove Meningioma
Susan saw a local neurosurgeon and got two additional opinions before emailing the Pacific Brain Tumor Center. After Dr. Barkhoudarian responded personally to her email with a phone call, she knew she wanted a surgeon who dealt with tumors like hers regularly.