Intraventricular Tumors
What are Intraventricular Tumors?
Intraventricular tumors are a diverse group of tumors that originate within the ventricles of the brain, which are fluid-filled spaces responsible for the production and circulation of cerebrospinal fluid (CSF). These tumors can occur in individuals of all ages, although some types are more commonly observed in specific age groups.
There are various types of intraventricular tumors, including ependymomas, choroid plexus tumors, central neurocytomas, subependymal giant cell tumors, and others. Each of these tumors arises from different types of cells within the ventricles, leading to distinct clinical presentations, characteristics, and treatment approaches.
Types of Intraventricular Tumors
Ependyomas
Ependymomas are one of the most common types of intraventricular tumors. They originate from ependymal cells that line the ventricles. Ependymomas can occur at any age but are more frequently diagnosed in children and young adults. These tumors can obstruct CSF flow, leading to increased intracranial pressure and symptoms such as headaches, nausea, vomiting, and visual disturbances. Surgical resection is the primary treatment for ependymomas, often supplemented with radiation therapy.
Choroid Plexus Tumors
Choroid plexus tumors arise from specialized cells that produce CSF within the ventricles. They are more commonly found in infants and children. Choroid plexus papillomas are typically benign, whereas choroid plexus carcinomas are malignant. These tumors can cause overproduction of CSF, leading to hydrocephalus and associated symptoms. Surgical resection followed by chemotherapy or radiation therapy is the standard treatment approach.
Central Neurocytomas
Central neurocytomas are rare tumors that primarily affect young adults. They arise from neuronal cells within the ventricles. These tumors are usually slow-growing and may cause symptoms such as headaches, seizures, and cognitive changes. Surgical resection is the primary treatment, and adjuvant therapies may be considered in cases with residual or recurrent tumors.
Subependymal Giant Cell Tumors
Subependymal giant cell tumors (SEGAs) are benign tumors that often develop in individuals with tuberous sclerosis, a genetic disorder. SEGAs arise from cells lining the walls of the ventricles. These tumors can lead to hydrocephalus and may cause neurological symptoms. Surgical resection or targeted therapy with mTOR inhibitors is typically employed.
Treatment of Intraventricular Tumors
Minimally invasive endoscopic keyhole surgery is now possible for most Intraventricular tumors
Intraventricular tumors include benign and malignant tumors that can be treated with unique, minimally invasive surgical approaches.
These tumors include gliomas, metastatic tumors, central neurocytomas, subependymal giant cell astrocytomas (SEGA), meningiomas, ependymomas, subependymomas, germinomas and germ cell tumors, choroid plexus papillomas and carcinomas and medulloblastomas (PNET).
The surgical approach is dependent on the tumor type, size and location specific to the ventricle.
Overview
The ventricles of the brain are fluid-filled structures that produce the cerebrospinal fluid that bathes the brain and spinal cord. The fluid is produced by the choroid plexus and has no “off switch.” Hence, tumors can block flow regionally, resulting in build-up of fluid and pressure.
There are four ventricles, with the lateral ventricles draining into the third ventricle through the Foramen of Munro. The fluid then flows through the cerebral aqueduct (of Sylvius) into the fourth ventricle where it exits the inside of the brain to circulate around the brain and spinal cord before being absorbed back into the blood stream.
Symptoms
Symptoms of these tumors/cysts can vary depending on their type and location amongst the ventricular system. Typical symptoms include headaches, vision loss or double vision, memory loss, imbalance, swallowing difficulties or hoarse voice.
These symptoms can take years to develop, but can worsen suddenly, progressing to altered mental status and coma if left untreated.
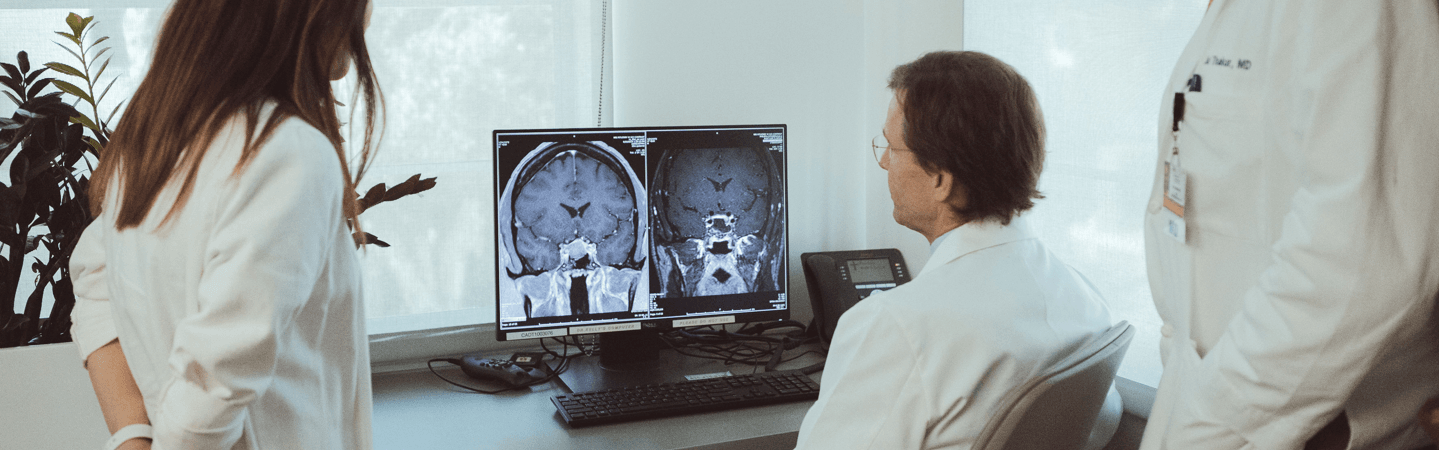
Diagnosis
As the treatment(s) of these lesions vary greatly on the diagnosis, numerous tests may be necessary prior to surgery. Typical imaging studies include magnetic resonance imaging (MRI) or computer tomography (CT) scans of the brain.
Fiber tractography MRI (DTI) is helpful to assess key neural fibers as well as surgical approach. The cerebrospinal fluid (CSF) may need to be analyzed via a lumbar puncture (spinal tap) if deemed safe. In specific situations, surgical biopsy may be necessary prior to definitive therapy.
Treatment
In many cases, small tumors can be observed. Often, however, a diagnosis is necessary and surgical biopsy or resection is warranted. For small tumors in the lateral and third ventricles, direct endoscopic biopsy and resection is possible. However, for larger tumors, a brain-port is helpful for better tumor access and control.
For 4th ventricle tumors, a suboccipital approach is utilized, with endoscopic assistance when necessary. Occasionally, an endoscopic third ventriculostomy is necessary to treat the hydrocephalus while a diagnosis or definitive adjuvant therapy is prepared.