
Surgery for Sleep Apnea
Understanding Sleep Apnea
What is Sleep Apnea?
Sleep apnea is a prevalent sleep disorder characterized by pauses in breathing or shallow breaths during sleep. These interruptions can occur multiple times per hour, leading to fragmented sleep and a range of associated health complications. The most common type of sleep apnea is obstructive sleep apnea (OSA), where the airway becomes blocked or collapses during sleep, often due to relaxed throat muscles. Central sleep apnea (CSA) is less common and involves a failure of the brain to signal the muscles to breathe. Mixed sleep apnea, as the name suggests, combines elements of both obstructive and central sleep apnea. These disruptions in breathing not only impair sleep quality but can also contribute to various health issues, including daytime fatigue, cardiovascular problems, and cognitive impairment. Fortunately, medical and surgical interventions can offer effective solutions for individuals with sleep apnea, targeting the underlying causes to improve breathing and restore restful sleep.
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea (OSA) is a sleep disorder characterized by repeated episodes of partial or complete airway obstruction during sleep. This leads to disrupted sleep and reduced oxygen levels in the blood. OSA occurs when the muscles in the throat relax during sleep, causing the airway to narrow or collapse. As a result, breathing is repeatedly interrupted or stopped entirely for brief periods, known as apnea events. These events can last from a few seconds to over a minute and may occur hundreds of times per night. The main features of OSA include:
- Loud, chronic snoring punctuated by periods of silence when breathing stops
- Gasping, choking, or snorting sounds as breathing resumes
- Excessive daytime sleepiness due to fragmented, poor-quality sleep
- Morning headaches, dry mouth, and sore throat upon waking
OSA can range from mild to severe, based on the apnea-hypopnea index (AHI), which measures the number of apnea and hypopnea (partial airway obstruction) events per hour of sleep. Severe, untreated OSA increases the risk of serious health problems like high blood pressure, heart disease, stroke, and type 2 diabetes. While OSA can affect anyone, certain factors increase the risk, such as being overweight or obese, having a large neck circumference, being male, and increasing age. Proper diagnosis through a sleep study and effective treatment are important for managing OSA and preventing associated complications.
Traditional Treatment Methods
Traditional treatment methods for obstructive sleep apnea (OSA) include CPAP therapy, lifestyle changes, and various surgical options. CPAP (Continuous Positive Airway Pressure) is the most common treatment, involving a machine that delivers a constant stream of air through a mask to keep the airway open during sleep. While effective, many patients find the mask uncomfortable and struggle with compliance.
Lifestyle changes, such as weight loss, avoiding alcohol and sedatives, and sleeping on your side, can also help reduce OSA symptoms.
For those who do not respond to CPAP or lifestyle modifications, surgical options may be considered. Surgeries for OSA include uvulopalatopharyngoplasty (UPPP), which removes excess tissue from the throat, and maxillomandibular advancement (MMA), which repositions the jaw to enlarge the airway. Each treatment has its benefits and limitations, and the choice of therapy depends on the severity of OSA and patient-specific factors.
Introducing Inspire: Mask-Free Sleeping
Surgery to implant the Inspire device for obstructive sleep apnea (OSA) offers an alternative for individuals who struggle with CPAP machines. The Inspire device and CPAP machine are both treatments for obstructive sleep apnea (OSA), but they function differently. CPAP delivers a continuous stream of air through a mask, keeping the airway open during sleep. While effective, many patients find the mask uncomfortable and challenging to use consistently. In contrast, the Inspire device is a surgically implanted system that stimulates the hypoglossal nerve to maintain an open and unobstructed airway. This method does not involve a mask or airflow, making it a more comfortable alternative for those who struggle with CPAP compliance.
What is Inspire Surgery for OSA?

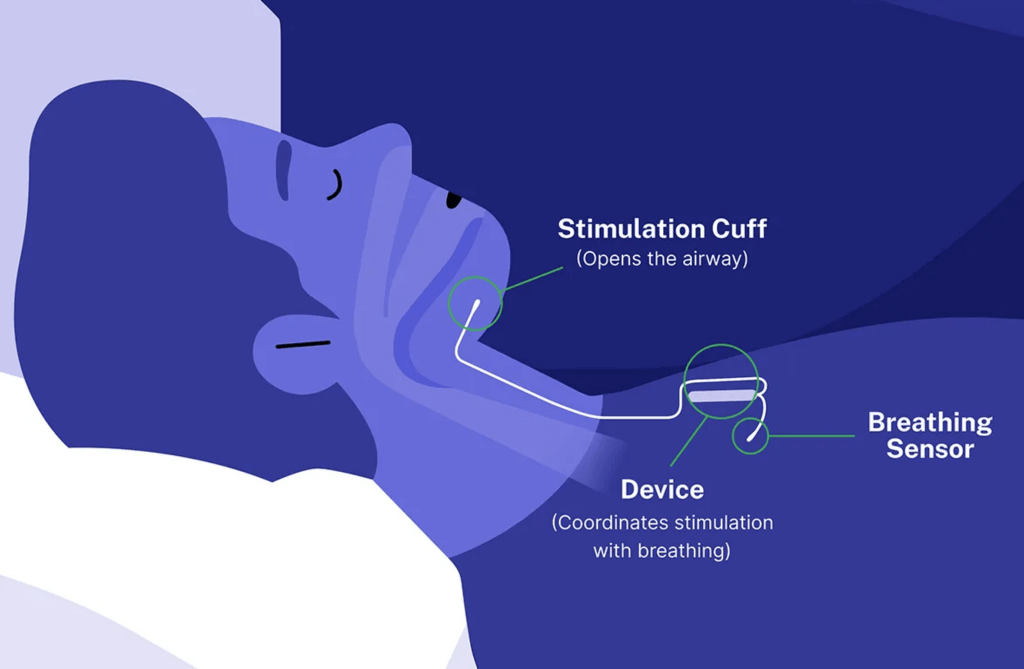
This minimally invasive surgery involves implanting a small device that works by stimulating the hypoglossal nerve, which controls tongue movement. The device helps keep the airway open during sleep, reducing apneas and improving sleep quality. Unlike traditional surgeries for OSA, Inspire therapy doesn’t involve removing tissue or altering the airway structure. Instead, it uses a gentle, rhythmic pulse to prevent airway collapse and eliminate or improve sleep apnea.
Patients activate the Inspire device each night using a handheld remote before sleeping. This targeted approach can be particularly beneficial for those who cannot tolerate CPAP masks and seek a more manageable long-term solution.
Benefits of Inspire Therapy
Inspire therapy offers significant benefits for those with obstructive sleep apnea (OSA) who struggle with CPAP machines. By providing targeted stimulation to the hypoglossal nerve during sleep, Inspire improves sleep quality and significantly reduces sleep apnea events. Patients often experience fewer interruptions in their sleep cycles, leading to more restful and restorative sleep.
Compared to CPAP, Inspire surgery tends to have increased compliance rates. CPAP requires wearing a mask throughout the night, which can be uncomfortable and difficult for many people. Inspire, on the other hand, involves a minimally invasive surgery for OSA to implant the device, which patients activate using a handheld remote before sleeping. This system eliminates the need for cumbersome masks and hoses, making it a more comfortable and convenient option. Consequently, patients are more likely to adhere to Inspire therapy, leading to consistent and effective management of their sleep apnea. Discuss Inspire therapy with your healthcare provider to see if it is suitable for you.
Who is a good candidate for Inspire therapy?
A good candidate for Inspire surgery typically includes individuals with moderate to severe obstructive sleep apnea (OSA) who have difficulty tolerating or complying with continuous positive airway pressure (CPAP) therapy. Specifically, candidates for Inspire therapy should meet the following criteria:
- Diagnosis of Moderate to Severe OSA: This is typically determined by a sleep study that measures the apnea-hypopnea index (AHI). Candidates usually have an AHI between 15 and 65 events per hour.
- Inability to Tolerate CPAP Therapy: Patients who have tried CPAP but find it uncomfortable, cumbersome, or ineffective are ideal candidates.
- Body Mass Index (BMI): A BMI of less than 32 is often required, though this can vary slightly based on specific guidelines and individual assessments.
- No Complete Concentric Collapse (CCC) at the Soft Palate: This is determined via a sleep endoscopy procedure. Patients with CCC may not benefit from Inspire surgery.
- Age and General Health: Typically, candidates are over 22 years old and in generally good health to undergo a surgical procedure.
Obstructive Sleep Apnea Treatment at PNI
CPAP machines are a first-line treatment for OSA however, they may not suit everyone’s lifestyle. For those with moderate to severe OSA, who are unable to tolerate CPAP, an implantable alternative called Inspire provides relief from OSA. The device works by delivering gentle pulses to airway muscles, keeping them open for regular breathing and sound sleep.
Patient outcomes with this device implant have been promising. 90% of bed partners report no snoring or soft snoring, and there is a 79% reduction in sleep apnea events. Remarkably, 94% of patients report that they prefer the implant over CPAP and would recommend it to others.
If you or a loved one are struggling with OSA, contact us to learn if you are a candidate for surgical implantation of Inspire.
Sleep Apnea Surgeon

Omid B. Mehdizadeh, MD, is an otolaryngology-head & neck (ENT) surgeon with particular expertise in voice, swallowing and airway conditions at Pacific Neuroscience Institute. He specializes in treating disorders of the larynx, voice box; swallowing; airway; ear and hearing; nose, throat and neck. A Los Angeles native, his career has spanned treating world-class opera and Broadway singers to surgical mission trips serving underprivileged and indigenous populations of Central America.
Clinic Location
11645 Wilshire Blvd., #600,
Los Angeles, CA 90025
310-477-5558
Written and reviewed by:
The Pacific Neuroscience medical and editorial team
We are a highly specialized team of medical professionals with extensive neurological and cranial disorder knowledge, expertise and writing experience.
Last updated: July 31, 2024
