Carotid Artery Disease
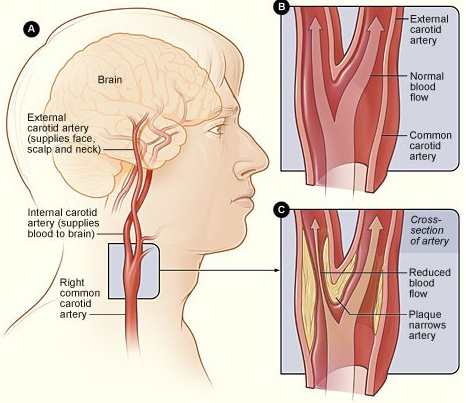
Carotid artery disease or carotid artery stenosis is the narrowing of the arteries in the neck caused by cholesterol deposition.
There are two carotid arteries, one on either side of the neck that transport oxygen-rich blood to the brain. Narrowing of these arteries is serious as it is a major cause of stroke. Many factors can lead to carotid artery disease including genetics, diet, and others. The cholesterol plaque can break off and block blood flow to the brain resulting in oxygen deprivation and causing a stroke. In addition, turbulent blood flow through a narrow artery can activate blood platelets, making them sticky. These sticky platelets can cause blood clots resulting in stroke as well.
Risk factors that lead to carotid artery disease include:
- Age: The arteries become more rigid with age.
- Obesity: Excess weight raises the chances of having high blood pressure and diabetes.
- Lack of exercise: A lack of exercise can worsen risk factors such as obesity, high cholesterol, and high blood pressure.
- Family history: Your risk is greater if another family member has carotid artery disease.
- Diabetes: Diabetes lowers your ability to process fats. People with diabetes are four times as likely to have carotid artery disease.
- Smoking: Smoking constricts blood vessels and lowers oxygen flow. It can lead to high cholesterol, increased heart rate, and high blood pressure.
- High blood pressure: Excess pressure on the arteries can cause them to weaken and become more prone to damage.
- High cholesterol: Having a high LDL and low HDL can increase fat in the blood stream.
- Poor diet: Eating foods that are high in fat, salt or sugar can increase your risk of carotid artery disease.
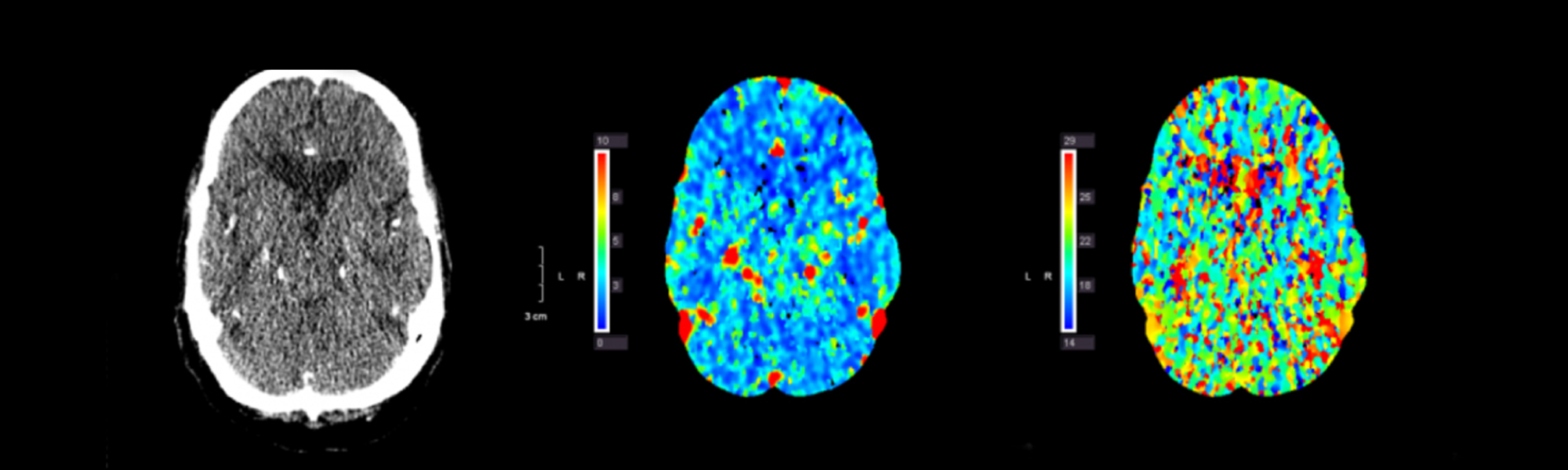
Diagnosis
There are several tests that can detect carotid artery disease.
- History & physical exam: A healthcare professional listens to the sound in your carotid arteries. This is not a guaranteed way to detect for disease.
- Doppler ultrasound imaging: A painless, noninvasive test in which sound waves bounce off of the arteries to check for blood flow and thickness of the arteries.
- Oculoplethysmography (OPG): Measurement of the pulse of the arteries in the back of the eye to indirectly check for blockages in the carotid arteries.
- Arteriography and digital subtraction angiography (DSA): A special dye is injected into the arteries and an X-ray of the carotid artery is taken. An invasive method like this carries some risk of stroke.
- Magnetic resonance angiography (MRA): Use of magnetic field and radio waves to provide detailed pictures of the arteries. An MRA can provide more data than an X-ray, ultrasound or CT scan.
Treatment
- Risk factor modification: The only risk factors that you can’t control are your genetics and your age. You can reduce your stroke risk by quitting smoking, maintaining a healthy weight, exercising daily, eating a Mediterranean diet, and controlling diabetes and hypertension.
- Medicine: Carotid artery narrowing causes blood platelets to become sticky and therefore medications that inhibit platelets (e.g. aspirin, clopidogrel) are an essential part of treating this disease. In addition, statin medications can help to lower plaque causing cholesterol.
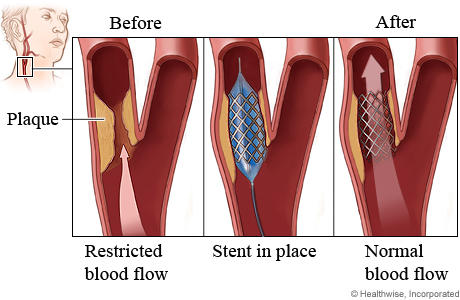
- Procedures: Carotid endarterectomy and carotid artery stenting are both very effective ways to prevent stroke in patients with carotid artery stenosis. Specific patient characteristics help to determine the more appropriate treatment for each individual.
- Carotid endarterectomy: This procedure involves the surgical removal of fatty build-up from the carotid artery.
- Carotid artery stenting: In this procedure, a wire mesh stent is placed in the carotid artery to “seal in” the cholesterol plaque and improve blood flow.
Carotid stenosis research: If your carotid artery stenosis has not caused a stroke or TIA, you may be eligible to participate in a new research study (CREST-2) aimed at determining whether medicines or procedures like stenting and surgery are better to treat your carotid artery disease. Contact us at the Pacific Stroke and Neurovascular Center if you would like to be evaluated for this trial.
Contact Us
The Pacific Stroke and Neurovascular Center’s state-of-the-art facilities are located at:
Providence Saint John’s Health Center
2125 Arizona Ave., Santa Monica, CA 90404
310-829-8319
Providence Little Company of Mary Medical Center Torrance
4201 Torrance Blvd., Suite 520, Torrance, CA 90503
424-212-5340
Providence Saint Joseph Medical Center
501 S. Buena Vista Ave., Burbank, CA 90505
818-847-6049
Providence Holy Cross Medical Center
15031 Rinaldi St, Mission Hills, CA 91345
818-847-6570