Endoscopic Endonasal Surgery
Video
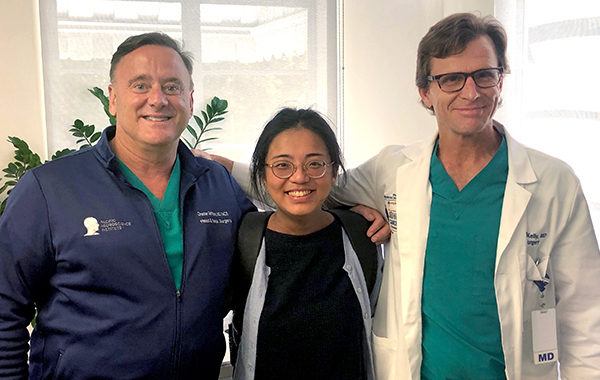
Treatment for a Benign Pituitary Tumor Causing Cushing’s Disease | Maple’s Story
After years of unexplained symptoms and frustration, Maple finally found the care she needed at Pacific Neuroscience Institute. Diagnosed with Cushing’s disease, caused by a benign pituitary tumor, she faced a challenging road ahead. But with the expertise of Dr. Daniel Kelly and the multidisciplinary team at PNI, Maple underwent a successful surgery that gave her back her health—and her life. Today, she’s thriving, having shed the symptoms that once controlled her. Her journey is a powerful reminder of how specialized care can truly transform lives.
https://www.pacificneuroscienceinstitute.org/blog/cushings-disease/treatment-for-a-benign-pituitary-tumor-gives-woman-her-life-and-body-back/
https://www.pacificneuroscienceinstitute.org/pituitary-disorders/conditions/pituitary-adenomas/cushings-disease/
https://www.pacificneuroscienceinstitute.org/pituitary-disorders/schedule-a-consultation/
Video
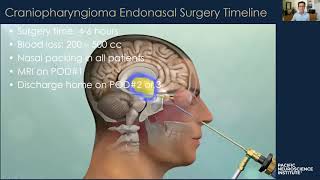
What is Cushing’s Disease? With Dr. Dan Kelly | A PNI Minute
Cushing's disease is a pituitary adenoma that causes the production of too much adrenocorticotropic hormone resulting in excess cortisol levels in the body. Listen to Dr. Daniel Kelly, MD, founder & director of Pacific Neuroscience Institute and one of the most experienced pituitary neurosurgeons in the world talk about Cushing's disease symptoms, diagnosis, optimal treatment, minimally invasive keyhole brain surgery and how this tiny tumor can lead to significant impairment of health.
https://www.pacificneuroscienceinstitute.org/pituitary-disorders/conditions/pituitary-adenomas/cushings-disease/
https://www.pacificneuroscienceinstitute.org/pituitary-disorders/people/daniel-kelly/
Pacific Pituitary Disorders Center
Ph: 310-582-7450
#cushingsdisease
#PNI
Video
Pacific Neuroscience Institute specialty care in Burbank CA
Pacific Neuroscience Institute physicians provide neurosurgery (brain and spine), neuro-oncology, elective neurovascular and emergency stroke services. Conditions treated at PNI-Burbank include brain tumor, pituitary disorders, facial pain, hydrocephalus, elective and emergency brain aneurysms and malformations, and stroke.
Providence Saint Joseph Medical Center in Burbank, CA, is a nationally renowned, award-winning hospital which strives to provide the best possible medical care to its patients and community.
Providence Saint Joseph Medical Center
https://www.pacificneuroscienceinstitute.org/about-us/providence-saint-joseph-medical-center-burbank/
Main: (818) 843-5111 | Neurosciences: (818) 847-6049
Video
Neurosurgical Fellowship Training at Pacific Neuroscience Institute
The Pacific Brain Tumor Center and Pacific Pituitary Disorders Center offers a 1-year neurosurgery fellowship in minimally invasive surgery for brain, pituitary and skull base tumors. Our clinical training program is focused on endoscopic endonasal and keyhole surgical approaches, neuro-endoscopy, pituitary tumor management and multimodality neuro-oncology treatments. The fellowship emphasizes operative and peri-operative patient management, outpatient evaluation of new patients and follow-up patients as well as clinical and anatomical laboratory research projects. The fellowship is integrated into the Saint John's Cancer Institute Surgical Oncology Fellowship.
Qualified applicants must have completed training in an ACGME-accredited neurosurgical residency program and be eligible for a California medical license.
https://www.pacificneuroscienceinstitute.org/resources/for-providers/fellowship-training-programs/#neurosurgery
310-582-7450
Video
Meningioma (Brain Tumor) Case Study | Dr. Daniel Kelly
Dr. Daniel Kelly, Neurosurgeon, Director and Founder, Pacific Neuroscience Institute, presents a case study of a 52 year old woman from New York who was experiencing progressive vision loss. After an MRI, she traveled to Los Angeles to receive minimally invasive keyhole surgery for a meningioma (brain tumor). Using a endoscopic, endonasal approach, the patient's tumor was removed via the nostril.
Pacific Neuroscience Institute is located at Providence Saint John's Health Center, Santa Monica, and Providence Little Company of Mary Medical Center, Torrance.
For more information call 310-582-7450
https://www.pacificneuroscienceinstitute.org/people/daniel-kelly/
https://www.pacificneuroscienceinstitute.org/brain-tumor/
https://www.pacificneuroscienceinstitute.org/
Resource
Pituitary adenomas in older adults (≥ 65 years): 90-day outcomes and readmissions: a 10-year endoscopic endonasal surgical experience
Thakur JD, Corlin A, Mallari RJ, Huang W, Eisenberg A, Sivakumar W, Krauss H, Griffiths C, Rettinger S, Cohan P, Barkhoudarian G, Araque KA, Kelly D. Pituitary. 2020 Sep 16.
Introduction
Longer lifespan and newer imaging protocols have led to more older adults being diagnosed with pituitary adenomas. Herein, we describe outcomes of patients ≥ 65 years undergoing endoscopic adenoma removal. To address selection criteria, we also assess a conservatively managed cohort.
Methods
A retrospective analysis of 90-day outcomes of patients undergoing endoscopic pituitary adenomectomy from 2010 to 2019 by a neurosurgical/ENT team was performed. Tumor subtype, cavernous sinus invasion, extent of resection/early remission, endocrinology outcomes, complications, re-operations and readmissions were analyzed. A comparator cohort ≥ 65 years undergoing clinical surveillance without surgery was also analyzed.
Results
Of 468 patients operated on for pituitary adenoma, 123 (26%) were ≥ 65 years (range 65–93 years); 106 (86.2%) had endocrine-inactive adenomas; 18 (14.6%) had prior surgery. Of 106 patients with endocrine-inactive adenomas, GTR was achieved in 70/106 (66%). Of 17 patients with endocrine-active adenomas, early biochemical remission was: Cushing’s 6/8; acromegaly 1/4; prolactinomas 1/5. Gland function recovery occurred in 28/58 (48.3%) patients with various degrees of preoperative hypopituitarism. New anterior hypopituitarism occurred in 3/110 (2.4%) patients; permanent DI in none. Major complications in 123 patients were: CSF leak 2 (1.6%), meningitis 1 (0.8%), vision decline 1 (0.8%). There were no vascular injuries, operative hematomas, anosmia, deaths, MIs, or thromboembolic events. Median length of stay was 2 days. Readmissions occurred in 14/123 (11.3%) patients, 57% for delayed hyponatremia. Intra-cohort analysis by age (65–69, 70–74, 75–79, ≥ 80 years) revealed no outcome differences. Cavernous sinus invasion (OR 7.7, CI 1.37–44.8; p = 0.02) and redo-surgery (OR 8.5, CI 1.7–42.8; p = 0.009) were negative predictors for GTR/NTR. Of 105 patients evaluated for presumed pituitary adenoma beginning in 2015, 72 (69%) underwent surgery, 8 (7%) had prolactinomas treated with cabergoline and 25 (24%) continue clinical surveillance without surgery, including two on new hormone replacement.
Conclusion
This study suggests that elderly patients carefully selected for endoscopic adenoma removal can have excellent short-term outcomes including high resection rates, low complication rates and short length of stay. Our experience supports a multidisciplinary approach and the concept of pituitary centers of excellence. Based on our observations, approximately 25% of elderly patients with pituitary adenomas referred for possible surgery can be monitored closely without surgery.
Introduction
Longer lifespan and newer imaging protocols have led to more older adults being diagnosed with pituitary adenomas. Herein, we describe outcomes of patients ≥ 65 years undergoing endoscopic adenoma removal. To address selection criteria, we also assess a conservatively managed cohort.
Methods
A retrospective analysis of 90-day outcomes of patients undergoing endoscopic pituitary adenomectomy from 2010 to 2019 by a neurosurgical/ENT team was performed. Tumor subtype, cavernous sinus invasion, extent of resection/early remission, endocrinology outcomes, complications, re-operations and readmissions were analyzed. A comparator cohort ≥ 65 years undergoing clinical surveillance without surgery was also analyzed.
Results
Of 468 patients operated on for pituitary adenoma, 123 (26%) were ≥ 65 years (range 65–93 years); 106 (86.2%) had endocrine-inactive adenomas; 18 (14.6%) had prior surgery. Of 106 patients with endocrine-inactive adenomas, GTR was achieved in 70/106 (66%). Of 17 patients with endocrine-active adenomas, early biochemical remission was: Cushing’s 6/8; acromegaly 1/4; prolactinomas 1/5. Gland function recovery occurred in 28/58 (48.3%) patients with various degrees of preoperative hypopituitarism. New anterior hypopituitarism occurred in 3/110 (2.4%) patients; permanent DI in none. Major complications in 123 patients were: CSF leak 2 (1.6%), meningitis 1 (0.8%), vision decline 1 (0.8%). There were no vascular injuries, operative hematomas, anosmia, deaths, MIs, or thromboembolic events. Median length of stay was 2 days. Readmissions occurred in 14/123 (11.3%) patients, 57% for delayed hyponatremia. Intra-cohort analysis by age (65–69, 70–74, 75–79, ≥ 80 years) revealed no outcome differences. Cavernous sinus invasion (OR 7.7, CI 1.37–44.8; p = 0.02) and redo-surgery (OR 8.5, CI 1.7–42.8; p = 0.009) were negative predictors for GTR/NTR. Of 105 patients evaluated for presumed pituitary adenoma beginning in 2015, 72 (69%) underwent surgery, 8 (7%) had prolactinomas treated with cabergoline and 25 (24%) continue clinical surveillance without surgery, including two on new hormone replacement.
Conclusion
This study suggests that elderly patients carefully selected for endoscopic adenoma removal can have excellent short-term outcomes including high resection rates, low complication rates and short length of stay. Our experience supports a multidisciplinary approach and the concept of pituitary centers of excellence. Based on our observations, approximately 25% of elderly patients with pituitary adenomas referred for possible surgery can be monitored closely without surgery.